What Is Hypovolemic Shock: Definition
Hypovolemic shock is an urgent medical condition, which occurs when a rapid decrease of the volume of the intravascular fluid–usually due to severe bleeding–results in inadequate perfusion of the peripheral tissues and, eventually, in multiple organ failure 1,43.
Hemorrhagic shock is hypovolemic shock caused by bleeding.
Typical symptoms and signs: a person “does not look right,” is anxious, has pale, cool and sweaty skin and weak pulse, is lethargic and may lose consciousness.
Treatment includes stopping bleeding, intravenous fluid infusion, oxygen and drugs.
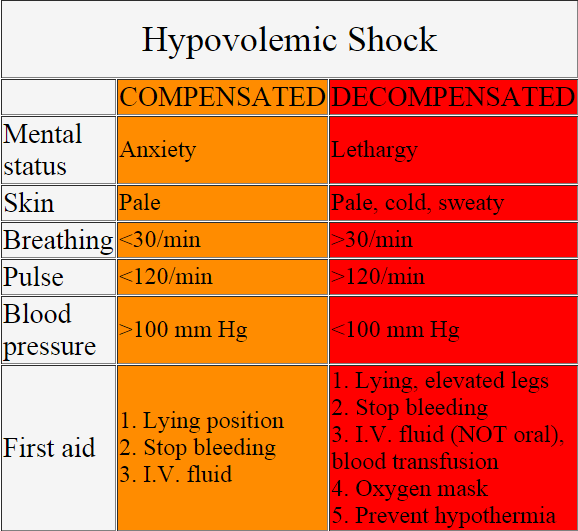
Table 1. Hypovolemic shock at a glance:
vital signs and first aid
Causes and Risk Factors
The most common cause of hypovolemic shock in adults is severe bleeding, and in children diarrhea 1.
Causes of hypovolemia:
- Loss of blood 1
- External bleeding: penetrating injury, heavy menstruation, scalp tear 1
- Gastrointestinal or rectal bleeding (blood in the stool):
- Rupture of the esophageal varices (in chronic alcohol abuse with liver cirrhosis)
- Esophageal tear due to violent vomiting, mostly in alcoholics (Mallory-Weiss syndrome)
- Rupture of hemorrhoids
- Aorto-intestinal fistula 1
- Bleeding peptic (gastric or duodenal) ulcer or gastric perforation (stomach cancer) or Meckel’s diverticulum 1,23
- Ulcerative colitis
- Ischemic colitis
- Intestinal perforation (for example, in diverticulitis)
- Iron toxicity 5
- Colorectal cancer (after age of 50)
- Bleeding disorders, such as hemophilia 23
- Other causes of internal bleeding:
- Spleen rupture in car/motorbike accidents 1
- Rupture of the aortic aneurysm or aortic dissection 1
- Rupture of hepatic hemangioma 19
- Retroperitoneal bleeding (anticoagulant therapy with warfarin or heparin in individuals with deep venous thrombosis) 3
- Fracture of the pelvis or femur 1
- Hemorrhagic pancreatitis
- Minor injuries in hemophilia
- Bleeding during or after surgery
- Pregnancy-related bleeding:
- Ruptured ectopic pregnancy 1
- Placenta previa 1
- Placental detachment (abruptio placentae) 1
- Uterine rupture 3
- Bleeding after delivery 2
- Blood donation
- Loss of blood plasma
- Severe burns affecting >15% skin surface 2,23
- Decreased water intake 23
- Water loss
- Excessive sweating
- Repeated vomiting
- Severe diarrhea: gastroenteritis caused by rotavirus in small children (stomach flu), cholera 2,3
- Excessive urination or polyuria:
- Diabetes mellitus 15, diabetic ketoacidosis 23
- Diabetes insipidus
- Diuretics
- Salt-wasting kidney diseases (polycystic kidney disease) 15
- Hypercalcemia 21
- Endocrine causes:
- Severe, acute thyrotoxicosis (“thyroid storm”) with high fever, excessive sweating and diarrhea 36
- Acute adrenal insufficiency (“adrenal crisis”) in acute Addison’s disease with polyuria, vomiting and diarrhea 42
- Second spacing: The fluid moves from the blood into the “second space” (the space between the cells, which is also called extracellular or interstitial space) and causes edema:
- Hyponatremia (a decrease in osmotic pressure of the blood results in a shift of water from the blood into the body cells)
- Congestive heart failure (blood pooling in the venous system and consequent escape of water into the interstitial tissue [edema] and a decrease of the blood volume in the arteries (arterial hypovolemia) 11
- In anaphylactic and septic shock, the permeability of the blood vessels increases, so some fluid escapes from the blood into the interstitial space 18
- Third spacing: Fluid accumulation in the body spaces where normally is no or only little fluid (the abdominal cavity, retroperitoneal space, lungs, pleural space, pericardial sac):
- Aortic dissection (blood pooling in the newly formed space in the aortic wall)
- Burns — fluid accumulation in the skin blisters 18
- Soft tissue trauma
- Pancreatitis — pancreatic enzymes and cytokines damage the blood vessels what results in the escape of fluid from the blood 15
- Peritonitis 15
- Pulmonary edema
- Pleural effusion 15
- Intestinal obstruction, paralytic ileus, volvulus 3
- A decrease of oncotic pressure of the blood plasma due to low blood protein levels and hypoalbuminemia can result in the escape of fluid from the blood into the body tissues and cavities:
- Kidney disease with nephrotic syndrome with anasarca [generalized edema]12
- Protein malnutrition [Kwashiorkor] can result in distended bellies in starving children 12
- Liver cirrhosis resulting in ascites — accumulation of the fluid in the abdominal cavity 13
- Protein losing enteropathy 23
- Ovarian hyperstimulation syndrome 20
- Sickle cell anemia with splenic sequestration, mostly in young children 28
- Systemic capillary leak syndrome 24
NOTE: Many authors use the term third spacing for both second as third spacing.
Differential Diagnosis
There are other types of shock and other conditions that may resemble hypovolemic shock:
- Distributive shock due to massive vasodilation with an increase in the volume of the intravascular space with insufficient volume of the existing blood to fill this space and therefore a drop of blood pressure
- Septic shock due to infection 7
- Toxic shock syndrome, mainly in women in which a tampon-associated infection with staphylococci or streptococci results in vasodilation, high fever and rash) 7
- Anaphylactic shock 7
- Neurogenic shock due to spinal cord injury above Th4 or Th6 5 (low blood pressure, no tachycardia, warm skin, paraplegia or tetraplegia, numbness 2
- Toxic shock (poisoning with nitroprusside, bretylium)
- Cardiogenic shock due to heart failure (myocardial infarction, arrhythmia, cardiomyopathy, heart valve disease) 7,27
- Obstructive shock:
- Cardiac tamponade (muffled heart tones, distended neck veins) 2,7
- Tension pneumothorax (displaced trachea, decreased breathing sounds on one side) 2,7
- Hemorrhagic pneumothorax
- Pulmonary embolism 27
- Arteriovenous malformations 2
- Vasodilation as a side effect of drugs, such as barbiturates, nitrates, opiates, antihypertensives (beta blockers, vasodilators) 7,25,26
- Temporary autonomic dysfunction:
- Orthostatic hypotension 9
- Vasovagal syncope 10
The term “relative hypovolemic shock” can be used when the volume of the circulatory system increases due to vasodilation, for example in neurogenic shock, and the volume of the blood remains the same but insufficient to perfuse peripheral organs.
Pathophysiology
Compensated Shock
Shock is compensated until the cardiac output (CO) and systolic blood pressure (BP) remain normal and thus manage to maintain proper perfusion of peripheral tissues.
- Baroreceptor reflex. Bleeding or other cause of fluid loss results in a drop of blood volume and hence blood pressure, which is detected by baroreceptors in the aortic and carotid arch. Baroreceptors activate the sympathetic system–sympathetic nerves, which release norepinephrine (noradrenaline) and adrenal medulla, which releases epinephrine (adrenaline)–, which results in the constriction of the peripheral blood vessels in the skin and increased heart contractility and heart rate. The brain, heart and kidney arteries have an ability of autoregulation, which means they can maintain adequate blood perfusion despite a gross reduction of the blood pressure (systolic BP 60-100 mm Hg). All these changes result in the redirection of the blood flow from the skin, muscles and gastrointestinal tract toward the heart, brain and kidneys.
- Fluid retention
- Atrial volume receptors sense the drop of the blood volume and stimulate the release of the antidiuretic hormone (ADH) from the pituitary gland, which reduces water excretion through the kidneys.
- Osmoreceptors in the hypothalamus detect the increase of blood osmolality and trigger the release of the ADH 8.
- Decreased perfusion of the juxtaglomerular apparatus in the kidneys stimulates renin >> angiotensin I >> angiotensin II and finally aldosterone release from the adrenal cortex, which causes the retention of sodium and hence water in the kidneys, which helps to maintain blood volume.
- Movement of fluid from intracellular and interstitial space into the blood.
- Bronchodilation and hyperventilation triggered by increased sympathetic activity results in increased oxygen delivery to the tissues.
References 1,13,23,38
Progressive or Decompensated Shock
Shock is decompensated when cardiac output and blood pressure drop to the point where they can not maintain proper perfusion of the tissues any more. This results in decreased oxygen delivery to the tissues and switch from aerobic to anaerobic metabolism, which results in lactate production and lactic acidosis.
Irreversible Shock
Shock is irreversible when the damage of the vital organs is so extensive that death cannot be prevented despite treatment. The patient can still survive up to three weeks after the onset of irreversible shock 32.
Table 2. Stages (Classes, Grades) of Hypovolemic Shock; Vital Signs |
||||
Compensated |
Decompensated |
|||
Stage 1 |
Stage 2 |
Stage 3 |
Stage 4 |
|
Blood volume loss |
<15% (< 750 mL) | 15-30% (750-1,500 mL) | 30-40% (1,500-2,000 mL) | >40% (>2,000 mL) (immediately life threatening) 2 |
Cardiac output |
Compensated by constriction of vascular bed | Lower | Lower | Lower |
Systolic blood pressure |
Normal | Normal | <100 mm Hg | <70 mm Hg |
Diastolic blood pressure |
Normal | Increased | Often not detectable due to narrow gap between syst and diast BP | |
Respiratory rate |
Normal | Increased (tachypnea) | >30/min | Pronounced tachypnea |
Heart rate |
Slightly increased but <100/min | >100/min | >120/min | >140/min |
Pulse |
Normal | Weak | Weak | Weak or absent |
Capillary refill |
Normal (<2 sec) | Delayed (>2 sec) | Delayed (>2 sec) | Absent |
Urine output |
Normal (>30 mL/hour) | 20-30 mL/hour | <20 mL/hour | Negligible |
Skin |
Pale | Pale, sweaty | Cool, pale, sweaty | Cool, extremely pale, sweaty |
Mental status |
Slight anxiety | Slight anxiety, restlessness | Confusion, agitation | Lethargy, coma |
Table 2 references: 2,38
Therapeutical/Physiological Classification of Hemorrhagic Shock
- MILD: Normal blood pressure
- MODERATE: Low blood pressure that responds to fluid replacement
- SEVERE: Low blood pressure that does not respond to fluid replacement test
- CRITICAL: >40% blood loss or brain or heart involvement (coma, bradycardia)
- Reference: 16
Early/First Symptoms
Clinical symptoms and signs may not be present until 10-20% of the total blood volume in adults or up to 30% in infants is lost.
- Thirst due to hypovolemia (hypovolemic thirst) can appear after 15% blood loss
- Nausea
- Anxiety, irritability, agitation, sleepiness, confusion
- Pale, clammy skin (in dehydration, especially in heat stroke, skin is initially dry and warm)
- Symptoms of bleeding: vomiting blood (hematemesis), blood in the stool (melena), blood in the urine, bruising, chest or back pain (rupture of the thoracic aorta), abdominal or flank pain (rupture of the abdominal aortic aneurysm, stabbing), vaginal bleeding outside of menstruation.
Early Signs
- Paleness, excessive sweating (diaphoresis)
- NOTE: in heat stroke, the skin would be dry and warm
- Dilated pupils
- Increased heart rate (tachycardia; may not occur early in patients who take beta-blockers)
- Weak, wide pulse, initially due to increased adrenaline release and subsequent peripheral vasoconstriction and increased diastolic blood pressure
- Blood pressure may not fall until about 20% blood (in infants 30%) is lost. Older people with high blood pressure or atherosclerosis may be in the stage of decompensated shock even if their blood pressure is at 120 mm Hg or above 16.
- Increased breathing frequency (tachypnea)
- Capillary refill time (CRT)
- >2 seconds in infants, children and adults (CRT in healthy, especially in old people can be prolonged in cold ambient)
- >3 sec corresponds to ~10% drop of blood volume
- Body weight is decreased in external bleeding and dehydration, but not changed in internal bleeding, septic, anaphylactic or toxic shock.
- Early signs of dehydration: poor skin turgor, sunken fontanelle in infants, decrease in body weight
- Signs of internal bleeding: abdominal tenderness, swelling, discoloration, guarding, bruising pattern of Grey, Turner sign and Cullen’s sign
- Signs of gastrointestinal bleeding: blood in the nose, mouth, throat or rectum (rectal examination).
NOTE: In infants, early symptoms and signs of hypovolemic shock are less obvious than in adults 23.
Late Symptoms
- Early symptoms plus the following:
- Dizziness
- Fainting
- Weakness
- Confusion
- Lethargy
Late Signs
- Early signs plus the following:
- Mottled, cyanotic skin
- Increase of tachycardia, bradycardia or arrhythmia
- Increased breathing rate (tachypnea: >30/min) or decreased breathing rate (bradypnea: <12/min) 2
- Capillary refill time (CRT) >5 seconds or absent
- Decreased body temperature (hypothermia)
- Low, “narrow” blood pressure (systolic pressure falls earlier than diastolic, because it is more dependent on blood volume; systolic blood pressure may not fall until 30% blood is lost).
- Decreased or absent urination (<20 mL/hour)
- Coma
References: 1,2,7,23,29,35
First Aid (ABC)
Check for airway, breathing, circulation and, if necessary, start with resuscitation (artificial breathing, heart massage).
- Do not move a conscious person or his/her head with a suspected spinal cord injury (most possible in head injury, direct blow to the spine, fall from the height, traffic accident).
- Move an unconscious person, including the one with a suspected spinal cord injury, into a recovery position. At least two other people should assist you, if possible, to provide minimal twisting of the neck and back.
- Call for an ambulance (USA, Canada: 911, UK: 999, Australia: 000, India: 102).
Stopping External Bleeding
- Wear gloves, if possible.
- If the person does not seem to have an injured spinal cord (intact sensation in the arms and legs), move him/her in a lying position with the bleeding part about 12 inches or 30 cm above the heart, if possible.
- Check the wound and remove free foreign objects (sand, cloth, etc.). DO NOT remove or move objects that are stuck in the wound, such as a knife or a sharp piece of wood).
- If possible, pull the edges of the wound together and fix them with a bandage
- Cover the wound with a gauze and apply pressure with the hands for 20 minutes to stop bleeding (if possible the injured person can do it) ; during this time do not check if the bleeding has stopped. If no gauze is available, use a part of the clothing or a clean plastic bag or bare hands (clean, if possible). If a gauze becomes saturated with the blood do not remove it but add another gauze over it. If the bleeding does not stop apply pressure with your fingers to one of the pressure points (behind the knee or in the groin, on the inner side of the elbow or below the armpit). There are different opinions about using a tourniquet on a bleeding limb: some doctors say not to use a tourniquet or use it as a last resort, others say use at least 2 inches (5 cm) wide tourniquet between the wound and the body until bleeding stops 14.
- If the person feels cold, cover him/her with a blanket.
- DO NOT give a person anything to drink or eat, even if he/she is severely thirsty.
- Reference: 33
First Aid in Suspected Internal Bleeding
Internal bleeding may not be visible; it can be suspected in high speed injuries, traffic accidents, falls from the height, after stabbing, etc.
- A person with a suspected internal bleeding who does not likely has a spinal injury should lie flat with the feet raised about 12 inches (30 cm) above the level of the heart.
- DO NOT give a person anything to drink or eat, even if he/she is severely thirsty 50.
Laboratory Tests in Hypovolemia
Initial Tests and Procedures
When internal bleeding is suspected:
- Auscultation:
- No lung sounds on one side in pneumothorax/hemothorax
- Diagnostic peritoneal lavage
- Ultrasonography or CT of the thorax or abdomen
- Nasogastric tube and gastric lavage and upper endoscopy
- Chest X-ray if perforated ulcer or hemothorax is suspected
- Colonoscopy
- Angiography
- X-ray of limbs, when fractures are suspected
- Pregnancy test, when ectopic pregnancy is suspected
- Central vein catheter
- Thoracic tube to drain hemothorax
- ECG can be done to exclude heart attack or other causes of cardiogenic shock.
- References: 4,31,40
Monitoring of Hemodynamic Changes
- ECG to exclude cardiogenic shock.
- Central Venous Pressure (CVP) <4 mm Hg (<5 mm water) indicates hypovolemia 35
- Pulmonary Artery Occlusion Pressure (PAOP) also called Pulmonary Wedge Pressure (PWP) or Pulmonary Capillary Wedge Pressure (PCWP) is usually decreased 38
- Cardiac Output (CO) is reduced 23.
- References: 23,35,38
Blood Tests:
- CBC in bleeding is initially normal.
- Hemoglobin (Hb) can be low in chronic bleeding, but not in the first hours of acute bleeding.
- Hematocrit (HCT):
- Normal up to eight hours after onset of bleeding. After 8-12 hours, the redistribution of the interstitial fluid into the blood occurs, so HCT and Hb fall.
- Increased in fluid loss without red cell loss:
- Dehydration (diarrhea, vomiting, polyuria, excessive sweating)
- Plasma loss (burns)
- Sodium (Na):
- Normal in bleeding (initially)
- Decreased in hypovolemic hyponatremia
- Potassium (K)
- Chloride (Cl)
- Blood Urea Nitrogen (BUN) can be increased in dehydration, gastrointestinal bleeding, rhabdomyolysis, urinary outlet obstruction or sepsis 17
- Creatinine: normal, except in renal failure 23,31
- Urea: normal, except in renal failure 31
- Glucose levels: initially hyperglycemia (gluconeogenesis, glycogenolysis due to increased epinephrine), later hypoglycemia (due to glycogen exhaustion) 38
- Bleeding time: prolonged in late shock
- Activated partial thromboplastin time (aPPT): prolonged in coagulation disorders 31
- Prothrombin time (PT): prolonged in coagulation disorders 31
- Arterial blood gases (ABGs):
- pH<7.3 = acidosis 31
- Respiratory alkalosis progressing to metabolic acidosis (due to lactic acidosis) 13
- Metabolic acidosis can also occur in severe diarrhea 23
- HCO3– (bicarbonate) is decreased in metabolic acidosis
- Base deficit increases (become more negative) with acidosis which increases with the extent of hypovolemia (mild base deficit: 2 to -5; moderate: -6 to -14; over -15) 30. Base deficit is usually expressed as a negative base excess (BE). So, base deficit can be used as a guide for fluid resuscitation.
Urine Tests
- Urine specific gravity is usually increased 23
- hCG (pregnancy test) to test for ectopic pregnancy 23
Treatment
The following is an overview of the usual procedures and it is not meant as treatment instructions.
1. Ventilation
In a decompensated shock, 100% oxygen should be given by a non-rebreathable facial mask 25.
2. Immobilization
Immobilization of the neck spine and limbs in a patient with trauma should be done before transport.
3. Transport
The patient should be transported to the hospital as soon as possible.
The first goal in treatment of hypovolemic shock is to correct hypotension 38.
4. Fluid Deficit Replacement
Fluid deficit replacement can start during transport 35,38,40. Fluids, which should be warmed, should be given via 2 large bore i.v. lines. The following fluids can be used 41:
- Crystalloids (3 liters are needed to restore 1 liter of lost blood).
- Isotonic saline (0.9% NaCl)
- Ringer lactate
- Colloids (1 liter is needed to restore 1 liter of lost blood):
- Hetastarch
- Pentastarch
- Albumin
- Dextran
- Blood products (when 2,000 mL crystalloids does not help):
- Fresh frozen plasma (FFP)
- Packed red blood cells (PRBCs)
- Whole blood transfusion
- Products to assist normal blood function:
- Tranexamic acid (decreases mortality)
- Recombinant human factor VIIa
- Prothrombin complex
NOTE: Using large amounts of fluid before surgery has been questioned lately 16.
5. Stopping Internal Bleeding
Internal bleeding can be reduced by certain drugs or stopped by an immediate surgery.
- Gastrointestinal bleeding 40:
- Intravenous H2 blockers
- Vasopressin (can have severe side effects)
- Somatostatin, octreotide
- Surgery
6. Medications
Vasoconstrictors–medications that increase blood pressure should not be given before hypovolemia has been corrected by fluids. There is insufficient evidence in using vasoconstrictors in improving survival in the acute phase of trauma 8.
Norepinephrine (Noradrenaline)
Norepinephrine is released from the nerve endings of sympathetic nerves. It stimulates alpha 1 and beta 1 receptors and causes peripheral vasoconstriction, increases heart rate and contractility and rises both systolic and diastolic blood pressure 32. Norepinephrine as a drug can be used in acute fall of the blood pressure.
Epinephrine (Adrenaline)
Adrenaline stimulates alpha 1 and beta 1 receptors. It causes peripheral vasoconstriction, increases heart rate and contractility and systolic blood pressure 32.
Other Possible Medications:
- Dopamine in high doses, which increases vasoconstriction (dopamine in low doses causes vasodilation) 16
- Phenylephrine
- Dobutamine
- Isoproterenol
- Milrinone
Complications
- Multiple Organ Dysfunction Syndrome (MODS)
- Lungs: Acute Respiratory Distress Syndrome (ARDS)
- Kidneys: Acute tubular necrosis resulting in acute renal failure
- Heart: heart attack (myocardial infarct)
- Brain: seizures (in hypovolemic hyponatremia and heat stroke)
- Blood: disseminated intravascular coagulation (DIC) due to hypothermia and acidosis
- Gastrointestinal tract: stress ulcers, ileus, ischemic bowel (“dead gut”), leaky gut syndrome, abdominal compartment syndrome
- Liver necrosis
- Limbs: gangrene
- Hypothermia (due to low tissue perfusion, cold intravenous fluids, cold environment)
- Hyperthermia (in heat stroke or sepsis)
- Hemorrhagic shock and encephalopathy syndrome in infants and children (rare) (high fever, seizures)
- References: 7,13,23,39
Prognosis
Prognosis of hypovolemic shock mainly depends on the volume of blood lost, the speed of fluid replacement and underlying health conditions.
- References
- Emedicine (Hypovolemic shock definition)
- Emedicine (Causes and stages)
- Diseasesdatabase (Associated conditions)
- Emedicine (Initial investigations)
- Emedicine (Iron toxicity and gastrointestinal bleeding)
- Emedicine (Causes of bleeding)
- Merck Manual (Shock pathophysiology)
- Asnjournals (Osmoreceptors)
- PubMed Central (Orthostatic hypotension)
- PubMed (Vasovagal syncope)
- Windle PE, Shick L, 2016 Perianesthesia Nursing Core Curriculum E-Book, p. 321
- Emedicine (Nephrotic syndrome)
- Ceuprofessoronline (Absolute and relative hypovolemia)
- Lee C et al, 2007, Tourniquet use in the civilian prehospital setting PubMed Central
- FPnotebook (Hyovolemic hyponatremia)
- PubMed Central (The Physiology Approach to Hypovolemic Shock)
- Lerma EV, Blood urea nitrogen (BUN) Emedicine
- Pcc.edu (Third spacing in shock)
- PMC (Rupture of hepatic hemangioma)
- Emedicine (Ovarian hyperstimulation syndrome)
- Merck Manual (Hypercalcemia and polyuria)
- Yournursingtutor (First, second and third spacing)
- Elsevierhealth (Diagnostic algorhytm)
- PubMed Central (Capillary leak syndrome)
- Hawaii.edu (Drugs side effects and hypovolemic shock)
- Drugs.com (Barbiturates toxicity)
- Ren X, Cardiogenic shock Emedicine
- PubMed (Splenic sequestration in sickle cell anemia)
- Ahajournals (Capillary refill time)
- PubMed (Base deficit)
- Emedicine (Hypovolemic shock investigations)
- Dynamicnursingeducation (Compensated, uncompensated and irreversible shock)
- Betterhealth.vic.gov.au (First aid in external and internal bleeding)
- Inhs.org (Manegement)
- LWW.com (Traumatic hypovolemic shock)
- Emedicine (Thyroid storm)
- Patient.info (Thirst)
- Upenn.edu (Evaluation)
- Aacnjournals (Abdominal compartment syndrome)
- Emedicine (Treatment)
- Emedicine (Hypovolemic Shock Management)
- Addisonian crisis –an emergency overlooked Apiindia.org
- Mhhe.com (Circulatory shock)