What is periosteum?
Periosteum [from Greek peri = surrounding; osteon = bone] is a fibrous membrane that covers the outer surface of the bones [1,16].
Periosteum Location
Periosteum covers all the bones, except the kneecap (patella) and certain small bones in the wrists, hands and feet, which are embedded within the tendons [16]. The periosteum also does not cover the cartilaginous parts of the bones in the joints 17,35. The periosteum that covers the skull is called pericranium.
Besides the periosteum, the bones are covered by two other membranes:
- Endosteum, which covers the inner surfaces (cavities) of bones
- Perichondrium, which covers the cartilage, except the articular cartilage in the joints
Structure (Histology)
The outer, fibrous periosteal layer consists mainly of the dense irregular connective tissue, made of superficial collagen (type I) and deeper elastin fibers, and rare connective tissue cells (fibroblasts) [16]. This layer also contains arteries, veins, lymphatic vessels and sensory nerves [16,31].
The inner, cellular or osteogenic periosteal layer, also called cambium, which has got the name from the cambium between the bark and wood of a tree, is in direct contact with the cortical bone; it consists of progenitor cells that develop into osteoblasts, which produce the bone tissue. The cambium layer is thickest in a newborn and thins with age [16,31].
Thickness
In growing individuals, the periosteum of the long bones is 70-150 micrometers (0.07-0.15 millimeters) thick; it is thicker toward the ends of the bones, and it thins with age [38]. The periosteum of the nasal bones is about 0.8-1.8 mm thick [32], and the alveolar periosteum (under the gingiva) is about 0.5 mm thick [39].
As a result of periosteal reaction due to an irritating bone or systemic disorder, the periosteum can become several millimeters thick [20].
Endosteum
Endosteum covers the inner surfaces of the long bones. The endosteum is thinner than the periosteum since it contains very few fibers.
Sharpey’s Fibers
Sharpey’s perforating fibers run from the periosteum through the bone to the endosteum and firmly attach both membranes to the bone [34]. They are thin (<40 micrometers) but strong fibers made mainly of collagen and elastin [34]. They are abundant at the sites of the ligament and tendon attachments to bones and in the alveolar bone, from which the teeth grow [34]. Sharpey’s fibers become stronger with activity and weaker with lower blood estrogen levels [34].
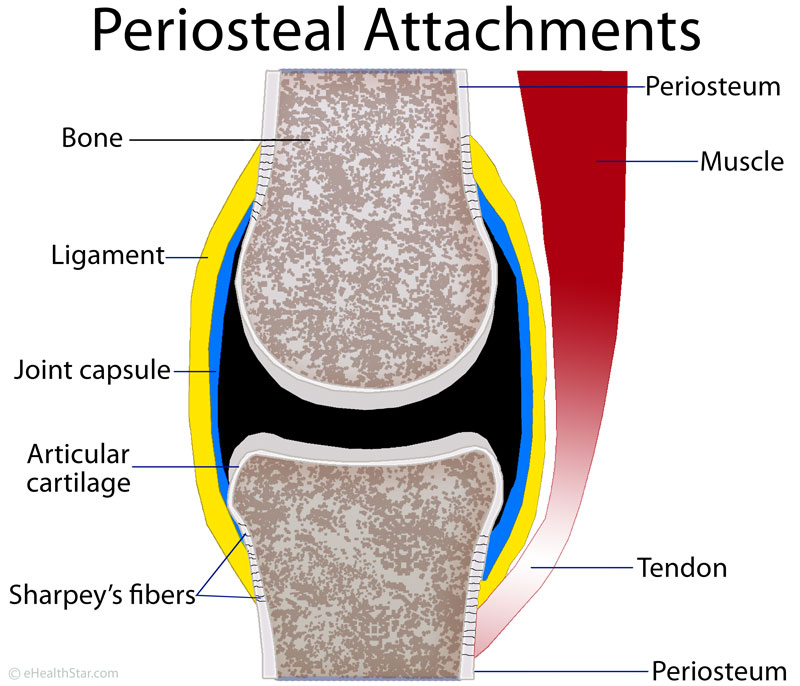
Picture 1. Periosteum location.
The periosteum covers the outer surfaces of the bones,
except in the joints, where the bone is covered by the cartilage.
Functions of the Periosteum
1. Attachment Sites for the Muscle Tendons and Ligaments
Certain tendons (bands that connect muscles to bones) and ligaments (which connect the bones in the joints) attach to the periosteum at the insertion sites, which are called entheses or osteotendinous or osteoligamentous junctions [16,35]. Some tendons and ligaments attach directly to the bones (not via the periosteum) [35]. In the joints, the periosteum continues into the articular cartilage and fibrous layer of the joint capsule [16].
Picture 2. Sharpey’s fibers connect periosteal attachments
(tendons, ligaments, joint capsule) firmly to the bone.
2. Nourishment of the Bones and Muscles
Periosteum contains periosteal arteries, which run within the outer periosteal layer and supply blood to the periosteum and outer third of the cortical bone [45]. Larger periosteal arteries run above the periosteum and communicate with the muscle arteries and contribute to the blood supply of the part of muscles adjacent to bones [45]. When the periosteum detaches from the bone due to injury, surgery or during obtaining periosteal grafts, it does not affect the blood supply to the muscles and it only minimally affects the blood supply to the bone, because the bone also gets blood from the arteries that run inside the bone [45]. The periosteum also contains veins, which collect the blood, and lymphatic vessels, which collect the lymph from the bones [1,16].
3. Bone Sensitivity (Innervation of Periosteum)
Sensory nerves in the outer, fibrous layer of the periosteum make it sensitive to tension and tearing [1,17]. Some nerve endings from the periosteum penetrate into the bone canals and thus make the bones sensitive to pain [44]. The periosteum also contains the sympathetic nerves, which regulate the diameter of the periosteal arteries and thus the blood flow through the periosteum [31].
Nerve fibers in the periosteum or bones of the skull and in the dura mater (the outermost brain membrane) may be involved in migraine pain [23]. Periosteal nerves contain substance P, which is involved in pain mediation [15].
4. Bone Growth and Repair
In children [1,16], the osteoblasts in the inner layer of the periosteum (cambium) produce new bone and thus enable the growth of the bone in the width or periosteal or appositional bone growth 1,16. Periosteal bone growth, to some extent, probably also occurs in adults [31].
After a bone fracture, the progenitor cells in the cambium develop into osteoblasts and chondroblasts that contribute to the bone repair and healing by forming a soft periosteal callus [1,16,48]. The bone healing potential of the periosteum decreases with age and is greater in long bones, such as the tibia, than in flat bones, such as the skull bones [16].
The periosteum may also contribute to bone wasting (resorption); for example, after a tooth loss, the alveolar bone under the gingiva shrinks [31].
Small bones, like wrist bones, that have only small amount of the periosteum, have spherical growth plates inside them [16].
In the growing males, low blood levels of estrogens are needed for periosteal bone expansion [18].
5. Periosteal Hinge
In certain fractures of long bones, the periosteum remains intact and acts as a hinge — it holds two pieces of the broken bone together [50].
Periosteum In Various Bones
1. Periosteum in the Skull (Pericranium)
Pericranium is the periosteum that covers the outer surface of the bones in the skull.
The inner side of the skull bones is covered by the outermost brain membrane or meninge called the dura mater, which has the periosteal layer, which is firmly attached to the skull bones, and the inner meningeal layer. At certain points, the two layers separate and form canals called cerebral sinuses or dural venous sinuses through which the venous blood from the brain flows.
Meningeal arteries, which supply blood for the dura mater, run between the periosteal layer of the dura mater and the skull bones, in the so-called epidural space [42]. A break of a meningeal artery, usually caused by a break of one of the skull bones, results in an epidural hematoma.
2. Periosteum In the Eye Orbit
The periosteum in the eye orbit is continuous with the dura mater [5]; it is loosely attached to the bone, so surgeons often elevate it when removing tumors in the orbit to avoid damage of the eye content [47].
A subperiosteal hematoma, usually in the roof of the orbit, can occur after a blunt trauma to the frontal area of the head (a fall or direct blow) [46].
3. Periosteum In the Spinal Vertebrae
The periosteum in the vertebrae is well innervated, which may be one of the reasons for pain during injection of anesthetic for epidural anesthesia [33].
Conditions Related to the Periosteum
A periosteal tear refers to a detachment of a part of the periosteum from the bone at the site where a ligament or tendon is attached to it [40]. It commonly occurs in football players when they suddenly twist a leg or foot. The main symptom is local tenderness and pain during stretching the affected tendon [40].
A subperiosteal hematoma or periosteal bruise is a collection of blood between the periosteum and the bone, usually due to a direct blow to the bone or bone fracture. Symptoms include local pain, a noticeable tender lump and skin bruise within minutes of injury.
Shin splints or medial tibial stress syndrome refers to an overuse injury of the shin area with pain in the lower two-thirds of shins triggered by exercise [6,11].
A periosteal ganglion is a ganglion cyst arising from the periosteum, mostly in adults [12,13,14]. It can develop after an injury and can cause pain, for example, in the wrist [14] or shin.
Periostitis refers to a periosteal inflammation and periosteal reaction to the formation of new bone or bone hypertrophy under the periosteum in response to bone irritation [2,3,17]. The terms are often used as synonyms. Symptoms may be absent or may include pain, tenderness and swelling of the affected limb [21,41]. Causes include shin splints, bone infection (osteomyelitis), vasculitis [26], benign tumors, fluorosis (especially in vertebrae) [20], cancer [21], chronic lung or liver disease and inflammatory bowel disease (IBD) [21]. Main causes in infants include congenital syphilis and physiological periostitis [41]. Diagnosis can be confirmed by X-ray, CT or MRI [3].
Picture 1. X-ray of a periosteal reaction (long arrow)
triggered by an osteoid osteoma (short arrow)
in the right thighbone (femur) of the 7-month old girl
(source: springer.com, Creative Commons license)
Periosteal necrosis–the death of a part of the periosteum–can result from burns [52], contact with bone implants [53] or osteomyelitis.
Periosteal Flaps and Grafts
Periosteal grafts can be used to treat defects in the connective tissue, bone, cartilage and muscles. This is possible because periosteal cells can differentiate into connective tissue cells (fibroblasts), bone cells (osteoblasts), cartilage cells (chondrocytes) or skeletal muscle cells (myocytes). An autologous periosteal graft, which is taken from the same person in whom the graft is used, for example, a galea-periosteum graft from the scalp [49] or a graft from the shinbone (tibia) can be used to treat:
- Knee cartilage defects caused by osteochondritis, osteoarthritis or injuries [24,25]
- A muscle hernia, for example, anterior tibial muscle hernia [19]
- Maxillary clefts [29] in infants
- The gingival recession defects in the gums [29]
- Frontal sinus defects [29]
- References
- Periosteum anatomy Britannica.com
- Ven D et al, 2002, Periosteal reaction with normal-appearing underlying bone: a child abuse mimicker
PubMed - Burgener FA et al, Periosteal reactions Bone and Joint Disorders: Differential Diagnosis in Conventional Radiology, 6th edition, 2006
- Daffner RH, Periosteal reactions Clinical Radiology: Essentials, 3rd edition, 2007
- Petruzzelli GJ, Orbit anatomy Emedicine
- Czarniecki M et al, Medial tibial stress syndrome Radiopaedia.org
- Bergman M et al, 2004, Asymptomatic Tibial Stress Reactions: MRI Detection and Clinical Follow-Up in Distance Runners Ajronline.org
- Gaeta M et al, 2005, CT and MR Imaging Findings in Athletes with Early Tibial Stress Injuries: Comparison with Bone Scintigraphy Findings and Emphasis on Cortical Abnormalities Radiology.rsna.org
- Anderson MW et al, 1997, Shin splints: MR appearance in a preliminary study Radiology.rsna.org
- Gaeta M et al, 2008, Diagnostic imaging in athletes with chronic lower leg pain PubMed
- Galbraith RM et al, 2009, Medial tibial stress syndrome: conservative treatment options PubMed Central
- Valls R et al, 1997, Diagnostic imaging of tibial periosteal ganglion PubMed
- Abdelwahab IF et al, 1993, Periosteal ganglia: CT and MR imaging features Radiology.rsna.org
- Blanco JF et al, 2003, Periosteal ganglion in a child Springer.com
- Grönblad M et al, 1984, Innervation of human bone periosteum by peptidergic nerves PubMed
- Dwek JR, 2010, The periosteum: what is it, where is it, and what mimics it in its absence? PubMed Central
- de la Roza G, Histology of bone Emedicine
- Bouillon R et al, 2004, Estrogens Are Essential for Male Pubertal Periosteal Bone Expansion Endojournals
- Jun-Ku L et al, 2012, Anterior Tibial Muscle Hernia Treated with Local Periosteal Rotational Flap – A Case Report Koreamed.org
- Rana RS et al, 2009, Periosteal reaction Ajronline.org
- Vandemergel X et al, 2004, Periostitis and hypertrophic osteoarthropathy: etiologies and bone scan patterns in 115 cases PubMed
- Amid PK, 2003, Surgical Treatment for Postherniorrhaphy Neuropathic Inguinodynia: Triple Neurectomy with Proximal End Implantation Spiegl.org
- Kosaras B et al, 2009, Sensory innervation of the calvarial bones of the mouse PubMed Central
- Niedermann P et al, 1985, Glued periosteal grafts in the knee PubMed
- Lu Y et al, 2002, Repair of cartilage defect of knee joints with free periosteal autograft PubMed
- Aries PM et al, 2005, Periostitis as the initial manifestation of systemic vasculitis Annals of the Rheumatic Disease
- Robertson MA, 2003, The relative effectiveness of periosteal pecking combined with therapeutic ultrasound compared to therapeutic ultrasound in the treatment of medial tibial stress syndrome type II Dut.ac.za
- Ogita M et al, 2008, Differentiation and Proliferation of Periosteal Osteoblast Progenitors Are Differentially Regulated by Estrogens and Intermittent Parathyroid Hormone Administration PubMed Central
- Mahajan A, 2012, Periosteum: A Highly Underrated Tool in Dentistry Hindawi.com
- Periosteal reaction University of Washington
- Augustin G et al, 2007, The periosteum – Part 1: Anatomy, histology and molecular biology Sveu?ilište u Zagebu, Medicinski Fakultet
- Tsai FC et al, 2010, Analysis of nasal periosteum and nasofrontal suture with clinical implications for dorsal nasal augmentation PubMed
- Bogduk N, Clinical Anatomy of the Lumbar Spine and Sacrum Clinical Anatomy of the Lumbar Spine and Sacrum, 4th edition, 2005
- Aaron JE, 2012, Periosteal Sharpey’s fibers: a novel bone matrix regulatory system? PubMed Central
- Benjamin M et al, 2006, Where tendons and ligaments meet bone: attachment sites (‘entheses’) in relation to exercise and/or mechanical load PubMed Central
- Animation: bone growth in width Mcgraw-Hill.com
- 2004, Bone and Bone Formation The University of Virginia
- Burr DB, 2012, Almost invisible, often ignored: periosteum, the living lace of bone Medicographia
- Eun-Hee C et al, 2011, Dimensional change of the healed periosteum on surgically created defects PubMed Central
- Bone membrane tear Sportnetdoc
- de Silva P et al, 2003, Physiological periostitis; a potential pitfall PubMed Central
- Meninges and meningeal spaces Inkling
- Middle meningeal artery Healthline
- Garcia-Castellano JM et al, 2000, Is Bone a Target-Tissue for the Nervous System? New Advances on the Understanding of Their Interactions PubMed Central
- Wheeles CR, Periosteal artery Wheelessonline
- Yazici B et al, 2011, Posttraumatic subperiosteal hematomas of the orbit in children PubMed
- Karaki M et al, 2006, Removal of an orbital apex hemangioma using an endoscopic transethmoidal approach: technical note PubMed
- Murao H et al, 2013, Periosteal cells are a major source of soft callus in bone fracture PubMed
- Grundmann T et al, 2004, Reconstruction of the frontal sinus with a calvarium split galea periosteum transplant after inflammatory complications PubMed
- Wheeles CR, Type III Supracondylar Frx Wheelessonline
- Recht MP et al, 2005, MRI of Articular Cartilage: Revisiting Current Status and Future Directions
Medscape - Ohara N et al, 2010, A case of lower-extremity deep burn wounds with periosteal necrosis successfully treated by use of allogenic cultured dermal substitute PubMed
- Wagner M, Internal Fixators: Concepts and Cases Using LCP and LISS, 2006




WhatHappening i’m new to this, I stumbled upon this I have found It positively helpful and it has helped me out loads. I hope to contribute & assist other users like its aided me. Great job.
Is periosteal massage useful in other injuries too or only for tennis elbow?
Possibly – you may want to ask an experienced physiotherapist.
Periosteal needling (its dynamic form) is a valuable diagnostic and therapeutic tool for physios and doctors, it telss you exactly that the very spot (or group of spots) on periosteum are responsible for pain or / and other disorders away from the needled region – this is the trick; it is usually not painful untill you press it with your finger and it gives you answers if you are communiacting with the mechanism of disorder…chcecked thousands of times, confirmed
greets from Poland