What is colorectal cancer?
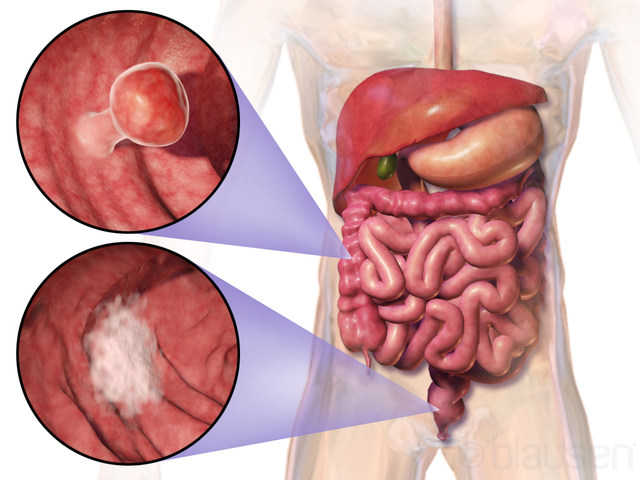
Colorectal cancer is cancer that grows in the large intestine (colon or rectum). Most colorectal cancers develop over several years from benign tumors called adenomatous polyps. Worldwide, colorectal cancer is the 2nd most common cancer in women and 3rd most common in men [9].
There are several types of colorectal cancer [1]:
- Adenocarcinomas (>95%)
- Carcinoid tumors
- Gastrointestinal stromal tumors
- Lymphomas
- Sarcomas
Picture 1. Two examples of colon cancer location
(source: Wikipedia, CC license)
Familial Adenomatous Polyposis
Familial adenomatous polyposis (FAP) is a rare genetic form of colorectal cancer in which hundreds of polyps can appear in the colon until adolescence and eventually (in 100%) develop into cancers [7]. In most cases, an affected person has one parent with the condition [7]. Treatment is by a surgical removal of the entire large intestine in early adulthood [7,8]. A patient with a total colon and rectum removal needs an ileostomy in order to excrete the stool.
Congenital hypertrophy of the retinal pigment, which can be detected by a slit-lamp examination, is commonly associated with FAP [8]. Other associated conditions include teeth abnormalities, bone overgrowths (osteomas), tumors of the connective tissue (fibromas) and epidermoid cysts in the legs, arms, face and scalp [8].
Causes and Risk Factors
The exact cause of colorectal cancer is not known.
Risk factors include [2]:
- Family history of colorectal cancer, including familial adenomatous polyposis (FAP), hereditary nonpolyposis colon cancer syndrome (HNPCC or Lynch syndrome) and Turcot syndrome
- Age over 50 [2]; the non-genetic type of colorectal cancer can, rarely, appear before 50 [25]
- A personal history of colorectal cancer or polyps (adenomas)
- Inflammatory bowel disease (Crohn’s disease, ulcerative colitis) [2]
- Being overweight or obese [2,13]
- Diabetes mellitus [26,27,28,29]
- Physical inactivity [2]
- Cigarette smoking (nicotine) [2]
- Excessive alcohol drinking [2,13]
- Exposure to X-ray radiation (radiation therapy) [24]
- Adult-attained height [24]
- Geographical location: the incidence is highest in Australia, New Zealand, United States and Western Europe (possibly associated with the Western diet) and lowest in Western Africa and some parts of Asia [9,25].
Is red meat a risk factor for colorectal cancer?
According to several systematic reviews of studies, there is some association between colorectal cancer and high intake (>100 g/day) of red meat [12,13,14,15,24] (beef [10,11], pork [11], veal or lamb [11]), organic meats (liver) or processed meats (>50 g/day) (smoked and cured meats, meat with added salt or other preservatives: hot dogs, ham, bacon, sausages, luncheon meats) [12,13,14,15,24]. In one 2010 study of a UK Dietary Cohort Consortium, low intake (<40 g/day) of red meat, poultry and fish was not associated with colorectal cancer [16].
There is currently INSUFFICIENT EVIDENCE to claim that the following are the risk factors for colorectal cancer:
- Night shift work [2]
- Asbestos exposure [24]
- Schistosoma japonicum (an intestinal worm) [24]
- Iron from meat (heme iron), animal fat, cheese, dietary sugars [24,25]
Symptoms and Signs
Early symptoms and signs [6,9]:
- Often no symptoms, but a doctor may palpate an abnormal mass during digital rectal examination if the tumor is within reach of the fingers
- Blood in the stool (usually red) and eventual paleness due to anemia due to chronic blood loss
- Constipation, diarrhea, narrow stools and a feeling you need a bowel movement that is not relieved by doing so (if the cancer is in the rectum)
- Pain in the lower left abdominal quadrant or rectum
Late symptoms and signs [9]:
- Fatigue
- Loss of appetite
- Unintentional weight loss
- Tenderness or a palpable mass in the lower left abdomen
- Enlarged liver
- Accumulation of the fluid in the stomach (ascites) in some individuals.
The average age at which people get colorectal cancer is 68 [9]. It usually takes 10-20 years for cancer to develop from a benign tumor called adenoma [9].
Diagnosis
A doctor who suspects that a person may have colorectal cancer can perform physical examination and investigations [3]:
- Digital rectal examination: a doctor can detect an abnormal mass in the rectum with the fingers
- A test for blood in the stool (fecal occult blood test)
- X-ray with barium enema
- Colonoscopy — an investigation of the large bowel using an endoscope, which is a tube with a camera and light on the end. A biopsy–taking few pieces of suspicious bowel tissue– is usually performed during colonoscopy; the obtained tissues are further investigated under the microscope (histological investigation).
- Capsule colonoscopy is available: you swallow a pill-like camera, which takes pictures when passing through your colon. Sensitivity for adenomas greater than 6 mm is 84-89% [23].
- CT colonography (virtual colonoscopy)
Blood tests are not used for the diagnosis of colorectal cancer but can be used to evaluate the severity of the disease.
Staging
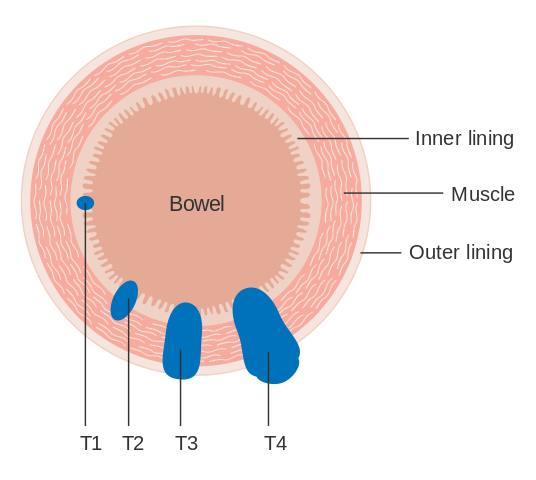
The TNM classification divides colorectal cancers according to the extent of a Tumor in the intestine, its spread to the Nodes (lymph nodes) and Metastatses (spread to other organs) [9]:
- Tis – In situ carcinoma; tumor involves only the mucosa (the intestinal lining)
- T1 – Cancer has grown through the mucosa and extends into submucosa
- T2 – Cancer has grown through submucosa and extends into the intestinal muscles
- T3 – Cancer has grown through the intestinal muscles and into outermost layers of colon but not through them
- T4a – Cancer has grown through the visceral peritoneum – the abdominal membrane that covers the intestine
- T4b – Cancer has grown through wall of colon and invades nearby tissues or organs
- N0 – No cancer in nearby lymph nodes
- N1a – Cancer cells found in 1 nearby lymph node
- N1b – Cancer cells found in 2-3 nearby lymph nodes
- N1c – Small deposits of cancer cells found in areas of fat near lymph nodes, but not in lymph nodes themselves
- N2a – Cancer cells found in 4-6 nearby lymph nodes
- N2b – Cancer cells found in 7 or more nearby lymph nodes
- M0 – No distant spread seen
- M1a – Cancer has spread to 1 distant organ or set of distant lymph nodes
- M1b – Cancer has spread to more than 1 distant organ or set of distant lymph nodes or has spread to distant parts of the peritoneum
Picture 2. T stages of colon cancer
(source: Wikipedia, CC license)
Chart 1. Colorectal Cancer Stages |
|||
| STAGE | Primary Tumor (T) | Lymph Node (N) | Metastasis (M) |
| Stage 0 | Carcinoma in situ (Tis) | N0 | M0 |
| Stage I | Tumor may invade submucosa (T1) or muscles (T2) | N0 | M0 |
| Stage II | Tumor invades muscles (T3) or nearby organs (T4) | N0 | M0 |
| Stage IIA | T3 | N0 | M0 |
| Stage IIB | T4a | N0 | M0 |
| Stage IIC | T4b | N0 | M0 |
| Stage IIIA | T1-4 | N1-2 | M0 |
| Stage IIIB | T1-4 | N1-2 | M0 |
| Stage IIIC | T3-4 | N1-2 | M0 |
| Stage IVA | T1-4 | N1-3 | M1a |
| Stage IVB | T1-4 | N1-3 | M1b |
Chart 1 source: Emedicine [9] The colorectal cancer staging bases on the TNM classification described above the chart.
Differential Diagnosis
Diseases that can cause similar symptoms as colorectal cancer [22]:
- Internal hemorrhoids
- Crohn’s disease
- Ulcerative colitis
- Rectal abscess
- Hyperplastic polyps
- Nodular lymphoid hyperplasia
- Diverticulosis
Treatment
It is an abdominal surgeon that treats colorectal cancer.
For colorectal cancer stages I-III, practically the only curative treatment is a surgical removal of a tumor and a small part of the intestine around it [9]. When a tumor is located near the end of the rectum, it may not be possible to reconnect the two parts of the intestine after the tumor removal, so a colostomy (the opening of the colon onto the abdominal wall) is needed.
Radiation therapy and chemotherapy are usually used only in more advanced stages [4,9]. Chemotherapy can prolong survival time [17,20] or at least disease-free time [19] in individuals with advanced colorectal cancer. Commonly used chemotherapeutics include 5-fluorouracil (5-FU), capecitabine, tegafur, oxaliplatin and irinotecan [9].
Biological agents used in treatment of advanced cancer include bevacizumab, cetuximab, panitumumab, ramucirumab, regorafenib, ziv-aflibercept [9].
Prognosis
After surgical removal, cancer can return at the same or other site in the colon. In some, but not all, people, the cancer recurrence is accompanied by increased blood levels of carcinoembryonic antigen (CEA) in the blood — in this case colonoscopy is usually done to confirm or exclude the cancer [5,9].
Survival Rate
The approximate 5-year survival rates for colorectal cancer are [1]:
- Stage I: 95%
- Stage III: 60%
- Stage IV (metastases): 10%
Prevention
Factors that may help prevent colorectal cancer:
- Physical activity [13,24]
There is INSUFFICIENT EVIDENCE of the preventative effect of garlic, milk, fish, non-starchy vegetables, fruit or fish [13,21,24], dietary fiber, calcium, folate, selenium, vitamin D [18,24] or aspirin [9].
Summary
- Colorectal cancer in the early stages may cause no symptoms, so if you have a family history of the cancer, it is recommended that you have colonoscopy after age of 50 [23].
- If you are after 50 and you notice blood in the stool, go and check with a doctor for a colorectal cancer.
- Early treatment of cancer in stage I has an excellent prognosis.
- References
- What is colon/rectum cancer? American Cancer Society
- Colorectal cancer causes, risk factors and prevention American Cancer Society
- Colorectal cancer early detection, diagnosis and staging American Cancer Society
- Colorectal cancer treating colon/rectum cancer American Cancer Society
- Colorectal cancer, living as a colorectal cancer survivor American Cancer Society
- Colorectal cancer, symptoms and signs American Cancer Society
- Familial adenomatous polyps Genetic Home Reference
- Familial adenomatous polyposis Emedicine
- Colon cancer overview Emedicine
- Carr PR et al, 2016, Meat subtypes and their association with colorectal cancer: Systematic review and meta-analysis PubMed
- Aykan NF, 2015, Red Meat and Colorectal Cancer PubMed Central
- Sandhu MS et al, Systematic Review of the Prospective Cohort Studies on Meat Consumption and Colorectal Cancer Risk A Meta-Analytical Approach Cancer Epidemiology Biomarkers & Prevention
- The report on updated evidence for colorectal cancer was published in 2011, Colorectal (bowel) cancer World Cancer Research Fundation
- Pham NM et al, 2014, Meat Consumption and Colorectal Cancer Risk: An Evaluation Based on a Systematic Review of Epidemiologic Evidence Among the Japanese Population Japanese Journal of Clinical Oncology
- Chan DSM et al, 2011, Red and Processed Meat and Colorectal Cancer Incidence: Meta-Analysis of Prospective Studies PubMed Central
- Spencer EA et al, 2010, Meat, poultry and fish and risk of colorectal cancer: pooled analysis of data from the UK dietary cohort consortium PubMed
- Best L et al, 2000, Chemotherapy improves the survival of people with advanced colorectal cancer, but the adverse effects and impact on quality of life are not yet known Cochrane
- Asano TK et al, 2002, Dietary fibre for the prevention of colorectal adenomas and carcinomas Cochrane
- Figueredo A et al, 2008, Adjuvant therapy for completely resected stage II colon cancer Cochrane
- Roqué i Figuls M et al, 2009, Second-line chemotherapy may increase survival of patients with advanced or metastatic colorectal cancer that have failed a first chemotherapy treatment Cochrane
- Weingarten MAMA et al, 2008, Daily intake of 1 gr dietary calcium may have moderate protective effect on development of colorectal adenomatous polyps Cochrane
- Colon cancer differential diagnosis Emedicine
- Colon cancer workup Emedicine
- Bowel cancer risk factors Cancer Research UK
- Haggar FA et al, 2009, Colorectal Cancer Epidemiology: Incidence, Mortality, Survival, and Risk Factors PubMed Central
- de Bruijn KM et al, 2013, Systematic review and meta-analysis of the association between diabetes mellitus and incidence and mortality in breast and colorectal cancer PubMed
- Deng L et al, 2012, Diabetes mellitus and the incidence of colorectal cancer: an updated systematic review and meta-analysis PubMed
- Yuhara H et al, 2011, Is diabetes mellitus an independent risk factor for colon cancer and rectal cancer?
PubMed - Larsson SC et al, 2005, Diabetes mellitus and risk of colorectal cancer: a meta-analysis PubMed