What is a bone bruise?
A bone bruise is a localized collection of blood within the bone caused by a bone contusion 1,6.
Characteristics:
- Most common in the knee and ankle
- Joint pain, swelling
- Not visible on X-ray; an MRI required for diagnosis
- Treatment with splints and analgesics
- Recovery time: several months
What is a bone contusion?
A bone contusion is any compression injury of the bone, which is usually associated with a bone bruise.
What is a subperiosteal hematoma?
A subperiosteal hematoma is a collection of blood between the periosteum and the bone, which is also commonly referred to as bone bruise.
What is bone marrow edema?
Bone marrow edema is an area of changed density on the MR image that reflects either a traumatic bone bruise or a nontraumatic collection of the fluid within the bone.
NOTE: Bone bruise, bone contusion and bone marrow edema are often used as synonyms 6,8,9,10.
Types of Bone Bruise
- A. Intraosseous bleeding
- B. Subperiosteal hematoma
A. INTRAOSSEOUS BLEEDING
Intraosseous bleeding [intra = within; os = bone], which means the bleeding within the bone, is what is most commonly referred to as bone bruise and what is the main part of this article.
Medical Definition
A bone bruise is a localized collection of blood within a bone associated with a fracture of the inner, spongy part, but not the outer cortical layer of the bone, caused by an acute trauma 9,10.
Causes
A bone bruise can be caused by acute trauma due to:
- The impact of the two bones in the joint or
- Direct blow to the joint
Bone bruises are common in football, soccer, basketball and hockey players, in those who practice martial arts, in runners who run on hard surfaces; other common causes are falls and car accidents 1,6.
Symptoms and Signs
- Swelling of the joint and, sometimes, one or more skin bruises, which do not result from a bone bruise but from injured ligaments, tendons, muscles and skin
- Pain in the affected joint, which persists after the skin bruise ceases
- References 6,10
Bone Bruise In the Knee
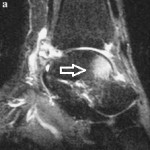
Picture 1. An MRI of a bone bruise in the knee
See the white patch in the upper tibia
(source: Physio-pedia.com, CC license)
Causes and mechanism. Sudden stop of running (deceleration), hard landing on a foot with slightly bent knee or direct side blow to the knee can result in the impact of the thighbone (femur) and shinbone (tibia) in the knee, what can cause a bone bruise in the lower part of the thighbone (lateral femoral condyle) and/or in the upper part of the shinbone (tibial plateau). Such an injury is often associated with a rupture of the anterior cruciate ligament (ACL), or medial (MCL) or collateral ligament in an athlete’s knee 1,6.
Pain and swelling arise from an injury of the soft tissues in the knee joint and not from a bone bruise 6.
Healing time. Most bone bruises associated with the anterior cruciate ligament rupture heal in 60 days, but the healing time may be as long as 2 years 10,30,41.
Recovery time. Most athletes who suffer from anterior cruciate ligament injury return to full sports activities within 6 months 6. The presence of a bone bruise does not seem to affect the recovery time 6.
Patella Dislocation and Bone Bruise
Side (lateral) dislocation of the patella can cause a bone bruise in the thighbone (in the lateral femoral condyle) and at the bottom of the patella 6.
Bone Bruise In the Ankle
A bone bruise in the ankle (in the lower part of the tibia or/and in the talus bone) can occur after an ankle sprain (supination injury after landing on an outward rolled foot with the outer edge of the foot bearing weight) 1. Pain after an ankle sprain usually ceases after 4-6 weeks; the presence of the bone bruise usually does not add to the pain and does not prolong the recovery time, which is about 3 months 28. In some individuals, a deep ankle pain during or after exercise may persist for some time. On an MR image, a bone bruise in the ankle can sometimes be seen even after 17 months, though 28.
Picture 2. An MRI of a bone bruise in the ankle
A white area in the back of the talus bone
(source: Physio-pedia.com, CC license)
Other Common Sites
Other common sites of bone bruise:
- Heel bone (calcaneus) after landing on the heels; partial weight-bearing for about 4 months may be required 32
- The ball of the foot 33
- Calf bone (fibula) in the part closer to the knee 18
- Hip (the femoral head) 5
- Pelvic bones: the ileal or pubic bone 34
- Shoulder blade (scapula)
- Shoulder: the head of the long bone (humerus) in the arm 38
- Elbow
- Wrist bones (especially the hamate) 37
- Spine (vertebra) 31
Types of Intraosseous Bleeding Based on MRI
Type 1: Reticular Bone Bruise
A reticular bone bruise is limited to the spongy part of the bone (medullary bone), is distant from the cortical bone and not connected to the joint surface; it is usually mild and scarce 25.
 |
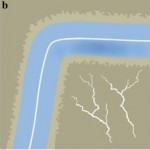 |
Picture 3. Reticular bone bruise in the ankle
a) An MRI of a reticular bone bruise in the front of the talus bone (arrow)
b) Bone cracks in the medullary but not in cortical bone
dark grey = medullary bone; light grey = cortical bone
blue = cartilage; white = joint space
(source: PubMed Central, CC license)
Type 2: Geographic Bone Bruise
A geographic bone bruise is bigger and denser than a reticular bruise and situated closer to the cortical bone; it can bulge into the joint space (see Picture 4) 25.
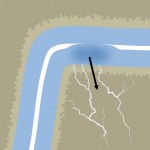
Picture 4. Geographic bone bruise
Dark grey = medullary bone; light grey = cortical bone
blue = cartilage; white = joint space
(source: PubMed Central, CC license)
Picture 5. An MRI of a large geographic bone bruise in the knee
(the large white area in the lateral femoral condyle)
(source: Physio-pedia.com, CC license)
Type 2a: Osteochondral Fracture
When a geographic bone bruise communicates with a joint, it is called osteochondral fracture 6. The damaged cartilage may need up to 1-2 years to heal 6.
Type 3: Impaction Bone Bruise
After an impact of the two bones in the joint, for example, the tibia and femur in the knee, a depression of the articular surface and bone bruises on the both bones can form; this is called a “kissing contusion” 9.
Picture 6. An MRI of a kissing contusion in the knee.
The upper bone bruise is in the thighbone (femur) and the lower in the shinbone (tibia)
(source: Orthopaedicsone, CC license)
Diagnosis
An X-ray can detect the real bone fracture but NOT an intraosseous bleeding (bone bruise within the bone) 25.
A CT also cannot detect intraosseous bleeding 25.
MRI
Currently, only magnetic resonance imaging (MRI) can detect bruises within the medullary bone:
- T1-weighted MRI shows a bone bruise as an area of decreased intensity 10.
- T2-weighted fat-suppressed MRI or MRI with Short T1 Inversion Recovery [STIR] sequences shows the area of increased intensity 10.
A bone bruise can be detected by an MRI as soon as 1-30 hours after an injury 41.
Differential Diagnosis
Conditions that can resemble a bone bruise:
- Overuse or stress or insufficiency fracture due to repetitive microtrauma
- Osteoarthritis
- Osteochondritis dissecans
- Subchondral cyst
- Periarticular bone infarction
- Bone tumor/cancer, lymphoma, multiple myeloma
- Bone inflammation (polyarthritis, reactive arthritis) or infection (bacterial arthritis, osteomyelitis)
- Osteopenia: scarce bone in malnourished individuals or those with anorexia nervosa
- Paget’s disease
- Gaucher’s disease
- Algodystrophy
- Intraosseous ganglion cyst
- Idiopathic transient bone marrow lesion syndrome
- Post-operative lesion
- Red marrow hyperplasia
- Intraosseous hematoma in individuals with bleeding disorders 26
- References 6,10
Treatment
First Aid:
- Elevate the affected limb.
- Put ice packs wrapped in the cloth over the affected joint for 5-10 minutes, few times a day for 1-2 days.
- Reference 37
Treatment Options:
- Rest, avoiding bearing weight on the affected limb; use of crutches or a cane as long as walking causes pain
- Splint (brace)
- Over-the-counter (OTC) painkillers and remedies to reduce pain and swelling
- Nonsteroidal antirheumatic drugs (NSAIDs), such as ibuprofen
- Physical therapy: nonbearing exercises to maintain full motion and prevent stiffness of the joint
- Avoiding smoking — nicotine delays wound healing 2
- Reference 6,10
There seems to be a lack of studies about the effectiveness of the following therapies on the bone bruise healing:
- Microcurrent therapy
- Kinesiology (kinesio) taping
- Acupuncture
- Vitamin A, C, K, and bromelain supplements
Healing and Recovering Time
Healing time (the time from an injury to the disappearance of a bone bruise on an MR image) for most bone bruises in the knee is about 2 months but can be as long as 2 years 10,30,41, and for the bone bruises in the ankle, it can be about 12 months or more 28. Reticular bone bruises heal fastest, followed by geographic and impaction bruises 6,10,30. Healing time is longer in older individuals and those with the knee osteoarthritis 30.
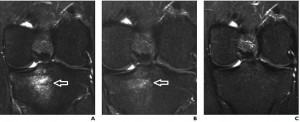
Picture 7. MRIs showing the healing of a bone bruise in the knee
(A) A bone bruise in the tibia soon after the injury
(B) After 3 weeks
(C) Complete healing after 9 weeks
(source: Physio-pedia, CC license)
Recovery time (the time to return to usual activities) can be shorter or longer than the bruise healing time and depends on the associated joint damage. The recovery time for most individuals with a bone bruise in the knee is shorter than 6 months and for those with a bruise in the ankle is about 3 months 19.
Complications
Possible complications of intraosseous bleeding:
- Stiffness of the affected joint 10
- Osteoarthritis, especially after a geographic bone bruise
- Avascular necrosis 10
B. SUBPERIOSTEAL HEMATOMA
A subperiosteal hematoma is a collection of blood between the periosteum and the cortical bone 1,20.
Subperiosteal Hematoma in the Shinbone (Bruised Shin)
A subperiosteal edema in the shinbone usually results from a direct blow to the shins, commonly in those who practice martial arts and in football players. Symptoms include pain, bluish discoloration of the skin (from a skin bruise) and tender swelling, which usually start to diminish in 2-3 days, but can often persist for several months 47. Investigations are usually not needed; in doubtful cases diagnosis can be confirmed by ultrasound, X-ray or CT 27. A bone bruise in the shinbone should not be confused with shin splints.
Treatment includes rest, elevation of the leg above the level of the heart, avoiding bearing weight on the leg, ice packs for 10-15 minutes several times a day for 1-2 days, and painkillers 24,47. A subperiosteal hematoma can get calcified, and the new bone tissue can form 39.
The Eye Orbit
A subperiosteal hematoma in the orbit (usually in the orbital roof) can appear days, weeks or even years after blunt trauma to the eye; other causes include weightlifting, violent vomiting, labor, sinusitis, panic attack or scuba diving 20,21. It most commonly occurs in young males 20. A spontaneous hematoma can appear in individuals with hemophilia, leukemia or scurvy 20.
Symptoms include protrusion of the eye and blurred vision that worsens over the days. Spontaneous healing is possible 29. Treatment may include intravenous antibiotics, steroids, aspiration or surgery 20.
The Skull
A subperiosteal hematoma in various skull bones can appear in newborns and rarely in older individuals with various bleeding disorders. Symptoms may include skin bruises anywhere in the body and a bulge on the scalp. A hematoma can resolve spontaneously, and if not, it can be punctured. If not treated within one month, it may lead to new bone formation (ossification), which requires surgical removal 23.
Other Sites for Subperiosteal Hematoma
- Pelvic bone (iliac or pubic bone): after a blunt or penetrating trauma 22
- Tailbone (coccyx) 40
Picture 8. Tailbone bruise (coccyx hematoma)
(source: Wikidot, CC license)
- Collarbone (clavicle) 35
- Ribs or breastbone (sternum) 4
- Forearm 37
What is a deep bone bruise?
The term deep bone bruise may be used for a bruise within the medullary bone (intraosseous bleeding) as opposed to a subperiosteal hematoma, which is a superficial bone bruise.
Bone Bruise vs Real, Stress and Occult Fracture
In a real bone fracture, both the cortical bone (the outer layer) and the medullary bone (the inner layer) are completely broken, and the bone parts are separated, which can be seen on an X-ray.
In a stress fracture due to repeated trauma, both the cortical and medullary bone are broken, but the bone parts on the both sides of the fracture do not split. A stress fracture can sometimes be detected by an X-ray, and if not, by an MRI 15.
In an occult bone fracture, both the cortical and medullary bone are broken, but the fracture line is so thin that it is not detected by an X-ray 3. The occult bone fracture that involves the bone and the cartilage and makes communication between a bone bruise and the joint is called osteochondral fracture 6.
In a bone bruise, only the medullary bone is broken, and the cortical bone remains intact. A bone bruise cannot be detected by an X-ray or CT but only by an MRI 3.
NONTRAUMATIC BONE MARROW EDEMA
Bone marrow edema is a term used to describe nonspecific changes of the density on the MRI image of the bone, which can include bone bruise (blood collection), true edema (fluid collection), or localized inflammation. Nontraumatic bone marrow edema can occur in various body parts from various reasons described below.
The Wrist and Hand
In rheumatoid arthritis, a bone marrow edema in the wrist is an early sign; it appears before rheumatoid factor in the blood 16 and is a bad prognostic sign 10,17.
The Foot
Bone marrow edema-like syndrome (BMES) of the foot and ankle can appear in younger patients with pain in the foot or ankle, without a known cause. Conservative treatment with splints may help.
The Hip
Nontraumatic bone marrow edema in the hip can be caused by:
- Avascular necrosis of the femoral neck 10
- Transient osteoporosis of the hip (TOH) in women in the 3rd trimester of pregnancy or in middle-aged men 10,11
- Main symptom: severe, disabling pain in the lateral thigh, no tenderness
- Can be treated solely with analgesics
- Heals completely after delivery
The Spine
In arthritis of the spine (spondyloarthritis), a bone marrow edema can be the first finding on an MRI 10.
Reactive Bone Marrow Edema
Reactive bone marrow edema refers to changes in the MR image caused by a response of the bone tissue to inflammation and may be caused by:
- Benign and malign bone tumors
- Osteoporosis
- Osteitis
- Osteoarthritis (edema is a bad prognostic sign)
- Osteonecrosis
- Transient bone marrow edema syndrome
- Ganglion cyst
- Complex regional pain syndrome
- Reference: 14
- References
- PubMed (Bone bruise overview)
- PubMed (Smoking and wound healing)
- MRIcenter.com (MRI, CT and X-ray of bone bruise)
- Researcgate (Subperiosteal hematoma in the ribs or sternum)
- PubMed (Bone bruise in the hip)
- PubMed Central (Athlete’s knee)
- American Journal of NeuroRadiology (Intraosseous hematoma)
- Sagepub (Bone contusion)
- BMJ (Kissing contusion in the knee)
- Diagnosticimaging.com (Bone marrow edema diagnosis and prognosis)
- PubMed Central (Transient osteoporosis or bone marrow edema of the hip)
- PubMed (Bone marrow edema)
- PubMed (Painful bone marrow edema syndrome)
- Gentili.net (Reactive bone marrow edema)
- Emedicine (Stress fracture)
- PubMed (Bone marrow edema as an early sign of rheumatoid arthritis)
- PubMed Central (Pathogenesis of rheumatoid arthritis)
- PubMed Central (Bone bruise of the knee)
- Natajournals (Ankle sprain)
- PubMed Central (Subperiosteal hematoma in the orbit)
- Informahealthcare (Subperiosteal hematoma in the orbit after an anxiety attack)
- PubMed (Traumatic subperiosteal aneurysm)
- PubMed (Subperiosteal hematoma in the skull bones in a newborn)
- ACSM’s Primary Care Sports Medicine, y.2007 (Subperiosteal edema in the tibia)
- PubMed Central (Types of bone bruises)
- American Journal of Neuroradiology (Intraosseous hematoma in an infant with factor VII deficiency)
- Ultrasoundcases.info (Ultrasonography of subperiosteal hematoma)
- Current Issues in Treatment of Osteochondral Defects, y.2013 (Osteochondral defect in the ankle)
- PubMed Central (Subperiosteal hematoma)
- PubMed (MRI of the knee in general practice)
- Researchgate.net (Bone bruise in the spine)
- PubMed (The heel bone (calcaneus))
- San Diego Running Institute (Metatarsalgia)
- NBCsports.com (Pelvic bone bruise)
- Netwellness.org (Bone bruise in the clavicle)
- Commonsportsinjuries.com (Shinbone bruise)
- Chiro.org (Forearm and wrist bone bruises)
- Healio.com (Bone bruise in the humerus head)
- Doctorslounge.com (Shin trauma not healing in 6 months)
- WebMD (Tailbone injury)
- Webcir.org (Radiography of occult bone trauma)







Pingback: Do Broken Bones Bruise Immediately
Pingback: How To Heal A Bruised Knee
Pingback: Should You Massage A Bruise
Pingback: Do Broken Bones Bruise
Pingback: Bruise On Shin For No Reason
Pingback: How To Treat A Deep Bruise Shoulder
Pingback: How To Cure Bruises On Knee
Pingback: Bruising At Top Of Legs
Pingback: Torn Mcl Bruising
Pingback: How To Heal A Bone Bruise On Shin
Pingback: Foot Bone Bruise Recovery Time
Pingback: Do Stress Fractures Bruise
Pingback: How To Reduce Bruise Pain
Pingback: What Is A Bone Bruise Shin
Pingback: What Is Bruising A Sign Of
Pingback: How To Treat A Hematoma Bruise
Pingback: Do All Broken Bones Bruise
Pingback: Can You Massage A Bruise Away
Pingback: How To Alleviate Bruise Pain
Pingback: What Does A Bone Bruise Look Like On Mri
Pingback: Are Bone Bruises Bad
Pingback: What Is The Treatment For A Bone Bruise
Pingback: How To Heal Bone Bruise Fast
Pingback: What Is A Bruised Meniscus
Pingback: Should I Massage Bruises
Pingback: Do I Have A Bone Bruise
Pingback: How To Heal A Bone Bruise On Elbow
Pingback: How To Ease A Bruised Knee
Pingback: Can You Bruise A Tendon
Pingback: Bruises On Knees Meaning
Pingback: What Do Bruised Knees Mean
Pingback: Will A Stress Fracture Bruise
Pingback: How To Diagnose A Bone Bruise
Pingback: Can You Bruise Your Pelvic Bone
Pingback: What Is A Bruised Knee
Pingback: Can Your Bones Bruise
Pingback: Can You Bruise A Bone In Shin
Pingback: How To Heal A Knee Bone Bruise
Pingback: Can Bones Bruise
Pingback: Why Are My Knees Always Bruised
Pingback: Can U Bruise A Muscle
Pingback: Can You Bruise A Bone In Elbow
Pingback: Will A Broken Bone Always Bruise
Pingback: Can U Bruise Your Bone
Pingback: Should A Massage Leave Bruises
Pingback: Indented Bruise On Shin
Pingback: Bruise On Shin For Months
Pingback: How To Heal A Bone Bruise Fast
Pingback: How To Heal A Bone Bruise
Pingback: Painful Lump On Shin No Bruise
Pingback: Permanent Bruise On Shin
Pingback: Bruise On Shin For No Reason
Pingback: How To Fix A Bone Bruise
Pingback: Permanent Bruise On Shin
Pingback: How To Treat Bruise Knee
Pingback: Bone Bruise Knee
Pingback: How To Remove Bruise On Knee
Pingback: Permanent Bruise On Shin
Pingback: How Long To Heal Bone Bruise
Pingback: Lump Under Bruise On Shin
Pingback: Bruised Knee From Falling On Concrete
Pingback: Raised Bruise On Shin
Pingback: Red Bruise On Shin
Pingback: Bruising Easily And Cuts Not Healing
Pingback: How To Heal A Heel Bone Bruise
Pingback: How Long Do Bone Bruises Hurt
Pingback: What Is Easy Bruising
Pingback: Knees Bruise Easily
A month and a half ago I tripped & fell flat on the side of my face on a wooden dock. Extreme pain, swelling & bruising occurred immediately, but was almost gone in 2 weeks. However, I still have a raised, hard bump about the size of a nickel on the upper cheek, lower eye orbit edge. It’s painful to slight pressure & has an occasional “stinging” sensation. No fracture seen by X-ray. Will this clear up on its own or should I see an orthopedist, a plastic surgeon, or what kind of doctor? I’m a woman & the bump is very noticeable.
Hi,
This information is very useful thank you.
I had a bike accident three months and injured my knee. Still painful after this time so went for an MRI that’s shows all is fine apart from inferior patella bone bruising. If this is showing up after this amount of time is it still important for me not to weight bear? I have been weight bearing now for maybe two weeks for short distances, I’m also back driving,would you suggest to stay on the crutches until this heals completely? Is driving ok? I also started swimming twice a week.. is this safe to do with this injury?
Thank you
I’m not a doctor and I can’t give any recommendation, so please ask your doctor. I would say that until you feel pain it’s maybe best to avoid exercise and also maybe weight bearing.
I am a mail carrier who walks about 13 miles a day. Have been having foot pain for over 2 months. Ortho dr ordered MRI after x-ray showed nothing. Came back as a subchrondal marrow edema. It is in the ball of my foot. Have shoe insert ordered but not sure how that will work with my job. What is your opinion?
Do you like your job?
Diagnosed with a heel bone bruise after a hard fall. It’s only been 3 weeks but the heel and area below my toes are still a bit swollen. The middle of foot is all bruised up. No attempts to walk on it, as it is too painful. Developed a DVT in calf after week one. I have an out of country trip I cannot cancel in 5 weeks. Are the chances slim that I will be able to walk a little by then?? Just want more opinions, thanks.
The doctor who gave you a diagnosis and who knows the extent of a bruise bone can answer this most reliably.
Hi. I recently got hit with a softball really hard on my right foot underneath my ankle. I went to the Dr and was diagnosed with bone contusion, xrays where negative. They advices me to use crutches for a few days but due to my job situation its hard for me to be on crutches so i ve been walking on my heel and dealing with the pain but is getting unbearable now. Can i use an orthopedic boot to help with the walking around? And how long do you think is going to take before i can return to playing sports?
Please listen to your doctor. X-ray cannot confirm/exclude bone bruise, but MRI can. Pain during walking suggest you you should not bear weight on that foot. If it is actually a bone bruise, it may take you weeks rather than days to be able to walk normally. By walking now you can make further damage and prolong the recovery period.
I understand. Can i wear an orthopedic boot instead of crutches though? Would that help the same as crutches stabilizing my foot and allowing me to atleast do some walking around at work? Or do i need to stay off my foot completely?
I can’t answer this.
Hi, I had a bone bruise diagnosed involving the bottom of my tibea and a bone in my ankle 7 months ago and I am still having trouble. My job involves a lot of walking and I am only now trying to return to work. The orthopedic specialist has suggested surgery to “clean it up”. I am really not sure if I want to do this as it will mean a couple of more months of healing time. He made it clear there were no guarantees with this op and I get the feeling he doesn’t know what else to do. Any thoughts?
You may want to ask for second opinion. Returning to the job that includes a lot of walking while still having pain may worsen the pain and prolong the recovery period. Maybe there is some small fracture or something else what would actually need surgical treatment.
I had the ankle injury for over 2 months now. In the first 3 weeks, the results of X-rays, CT scans and ultrasound were all negative. So I continued to put weight on my ankle and walk on it until one day it became too painful to do so. The doctor told me to do an MRI and I was diagnosed with bone bruise. I went to a orthopaedic specialist and he told me to put weight on it. After a day of walking, the ankle started bleeding again. I listened to my body and avoided weight for 4 weeks. I then went to another orthopaedic specialist for a second opinion and he also asked me to put weight on slowly. After a day of putting weight on, there was no bleeding but it turned purplish blue in colour and it got worse. It’s been two weeks off weight again after I put weight on. I have a purplish colour foot whenever I stand up for a period of time. It is quite depressing. Should I continue to be off weight? Why does the specialists keep asking me to put weight on. I’m not sure if it’s the right thing to do but it’s obvious that the ankle gets worse whenever I do it. When will the ankle stop going purple? Any idea how long it will take me to heal? How long should I be off weight on my ankle 🙁
In most cases, you should avoid weight-bearing when you have a bone bruise. Also, use your intuition. I strongly recommend you to read few serious articles about it and find a reliable doctor who will help you to treat this. Healing may take few months.
Thanks Jan. I hear red LED infrared light therapy will assist to heal the bone or fracture faster. Has anyone heard about it. Would it be constructive to shine LED light on the bruised bone area? I do have a LED light belt.
I believe your doctor (or at least someone knowledgeable about bone bruises) can answer this more reliably than I can.
I just checked and there are no DVT conditions on my leg.
How long should the bruised ankle bone be needing to be off weight typically?
I just wanted to get an estimation as to how long I should be on crutches.
Anyone, please comment.
It can be several months; I can’t be more specific. A doctor who knows how serious your bone bruise is can be the best judge.
This is to Aqua. It sounds to me like you may have a blood clot or vascular issue preventing proper blood flow when your foot is declined. This happened to me following a knee injury. I had to go back to the er 3 times before they finally checked for both. It turned out that I had 4 DVT’s & all my blood work came out with zero blood clotting markers. It was just from a fall that I didn’t think was that bad.
I agree that careful examination of tissues other than bone needs to be done.
Dawn and Jan, thanks for your comments. You have alerted me on the blood clot issue which I never thought of. Do you think I should go back and see my Orthopaedic Specialist or get a referral directly to a Hematologist to check it out?
An injury can cause a problem with local circulation in the foot, which can arise from the blood vessels, nerves or the surrounding tissues and not necessary from impaired blood coagulation (thrombosis). So, you may want to see your primary doctor or the one who diagnosed a bone bruise and they will guide you further.
Hi, I had a severe fall on my right hip a week ago and had to be taken to the hospital by ambulance. I was in horrible pain and could not stand up. No bones were broken. I could only get home with a walker. I see no improvement in my pain and still cannot put any weight bearing on that hip. I cannot move without a walker and still have sharp pain in the middle of my glute with each step. The pain also radiates into my groin area and the bottom of my glute. To get out of bed I have to manually lift my leg and still have shooting pains. I was told by my Doctor that I have bone bruises and possible torn ligaments and muscles. I am 65 years old and am a hairdresser. How long should it take me before I’m out of chronic pain and no longer have to use the walker. I cannot take anti-flammatories due to a bad stomach. I also cannot pain meds because I’m allergic to everything. I take tylenol extra strength. Also is there anything I can do to help speed up the healing of the bone bruise? I do not want to lose my business and am very depressed about this situation.
The doctor who told you that you have bone bruises can say what is the expected recovery time in your case. It can be several months for up to a year. The single most important thing you can do is rest (as little walking as possible). Other than that, you can ask the doctor if any surgical treatment could speed up healing.
I had a titanium rod, which had been in my tibia for 25 years, removed. It had bent and was very difficult to remove. It has been over 7 months and still have pain when walking, and some swelling in adjacent tissue. Can I expect a full recovery?
They would maybe need to do some imaging investigation (MRI) to find the cause of pain.
hey i dislocated my elbow in an arm bar in a Brazilian Jiu jitzu comp. there was no breaks or fractures of my bones just dislocated joint with some soft tissue soreness but i think i have bone bruising…i know its hard to say without seeing my elbow but what is the general diagnosis and type of bone bruising associated with this type of injury?
thanks
alex
A bone bruise can be confirmed by an MRI. There’s no way that a doctor can confirm or exclude bone bruise just by a physical examination. If the pain disappears in few weeks it’s unlikely that it is a bone bruise.
Hello it’s been 8 months since I fell and hit my shin on a concrete step resulting in a bone bruise. I still have blue purple and green discoloration in a six-inch area down front of my shin otherwise has healed completely as far as use of leg goes. (If I’m honest, it’s a bit tender when I press on it!) I never had any imaging done. Saw physician day 6….skin infection had developed, antibiotics cleared that up. He didn’t think imaging was needed since I was walking on leg. Any hope of normal skin color returning?
If the spot is tender it may didn’t heal yet. The persisting bruise may be due to constant underskin bleeding. I suggest you get this checked by a doctor.
1/19/17 I fell and bruised my hip. They said edema in the hip and femoral head. Anyway it is now 3/10/17 not in pain anymore is that a sign that the edema has resolved and can walk around. No pain on weight bearing.
The absence of pain does not already mean that the bone bruise has healed. It is your doctor who can tell you about walking.
I’ve had a knee bone bruise and a mcl sprain two months ago.
What kind of physical therapy exercises should I do?
Bone bruise and sprain need rest not exercise.
Hi, so I fell down the stairs and hit my shin very hard. It was numb for about nearly an hour and was very swollen and red. Now, it’s a little less than two weeks, and I just recently tripped and jammed it into a stool… It’s been on and off aching pain, stinging, tightness, and the bruise is clearly visible but all different shades. I’m not sure what to do. The doc said it was a contusion, but should it still be very tender to the touch?
To check if the bone is (partially) broken, you would need to have an X-ray.
I have a fairly extensive bone bruise on the lateral condyle on my left knee. It is already more than six weeks old, but I aggravated it 3 weeks ago by a bad decision to try to ski on it.
I find it is more comfortable if I walk on it than when I use crutches. After using crutches the knee is stiff and feels less stable. So if I “listen to my body” I want to walk on it (with care) instead of using crutches, but do you believe that I am just extending the recovery time by using it at all?
A doctor would probably recommend avoiding weight bearing. Light knee stretching exercises can prevent stiffness.
I have a shred tear of the peroneous brevis tendon along with a bruise of the dome of the Tallis bone I got by an inversion injury to my ankle. I was placed in a walking boot and 2 weeks later I had a forced dorsiflexion in the boot and bruised the other side of my Tallis bone. I have been in the boot for 2.5 months now. The tendons feels as though it is healing well but the Tallis bone is often still painful and my ankle still has edema if I walk on it much. As a physician I am forced to round on my patients in a wheelchair. My physician is trying to transition me to a figure of eight brace which causes me significant pain. Any thoughts on the persistent pain and edema with weight bearing and why my Tallis injury doesn’t appear to be responding to the non-weight bearing status when my tendon is?
Maybe there is another thing, besides bone bruise, such as stress fracture (hair fracture), that causes pain. Also, a bone bruise causing pain after 2.5 months is not that unusual. On the other hand, bone bruise or stress fracture alone should not cause visible swelling of the soft tissues. So, maybe there is some problem with the ankle joint.
You may consider to avoid walking completely for a certain period. An MRI can show a stress fracture and the status of the bone bruise.
Hi. I’m so glad I found this post. I started with severe pain in the inside of my knee Christmas 2015. Is had some pain when driving but it always went. I then said up and boy did it hurt. The result was horrific pain at the side of my knee. I had Physio, acupuncture, it didn’t help. I them had an MRI i had a cartilage tear in my right knee but also a massive bone edema where the two bones joined. The doctor said he could repair the tear but it wouldn’t improve the pain from the edema so he wasn’t happy to repair the cartilage as it wouldn’t improve my life. I was given a knee brace for 6months to wear to support the knee and seperate the bones. I have just chased it up as the side of the knee seems a lot better, rarely causes pain, but I now have a lot of pain especially on stairs in the knee itself. I’ve just chased up having the cartilage repaired to be told the surgeon said he wasn’t going to repair the cartilage. Not what I was told. I’m restricted at work and they aren’t happy I can’t do my full role. Neither am I. I’ve asked for a second opinion. How can there be a cartilage tear and they now won’t fix it. I could lose my job. Any advice or help would be much appreciated. I’ve waited 6 months expecting the cartilage to be repaired. Now I’m looking at just injections into the knee. What can’t they just repair the cartilage. Everything I’ve read shows bone edemas repair but not cartilage. I’m only 45 With a disabled child. I need to be fully mobile.
Did they tell you they will repair the cartilage later? You may want to avoid many steroid injections, because they can weaken the tissues within the knee joint. I encourage you to seek for 2nd opinion about the cartilage repair – also ask if delaying this repair would make it heal worse. At this point the pain may be still from both the bone edema and cartilage, though.
Hi. Thanks. Have asked for second opinion. First they said i need to wait for edema to go to then repair cartilage. Now they are saying no point repairing the cartilage, all they can offer are injections. My pain has decreased significantly. With paracetamol I am ok most of the time for normal everyday activities. Really worried if they don’t repair the cartilage what damage that wo then do to my knee.
I can’t reliably answer about cartilage, but ask some doctor specifically about it.
Dear,
Hope you are doing well.
I had a sport injury and was diagnosed as a Bone Bruise in Lateral Femoral Condyle in my left knee, it’s been around 3 weeks I have been using knee immobiliser and resting completely, I used to walk slightly daily to make sure the joint is use to for what it is for, on the other hand I have stiffness as well, I am unable to carry my leg straight or bend it fully. Although I can walk without pain. I am an Engineer and very much worried about my office routine & work, well is there any harm if I join my office and walk more without bracing ??
Nabeel, I can’t answer exactly, but avoiding weight bearing is very important in bone bruise healing. Ask the orthopedist about it. After some time the orthopedist will probably recommend an MRI to check if the bone bruise has healed or not. Healing time mainly depends on the severity of the injury.
Hey there, I was diagnosed with a bone bruise to my right lateral side of my ankle OCt.2014. The injury happened from me getting onto a bed and hitting a metal bedframe sticking out 2-4 inches in the middle of the bed, i had shooting pain going UP to the tailbone(stopping at the piriformis muscle), pain driving lifting ankle up and down, heel pain, calf pain, shin pain/muscle pain. Saw an Orthopedic gv me an injection and i felt the coldness rise UP all the way to the piriformis/stopping at the orbutar. It’s been 2 years and I am still having same pain, to now intensified and turned into Piriformis Syndrome. I have positive tinel signs. My groin area hurts constantly, I feel like I have done squats leg, thigh, calf always hot, just recently started to have palputations/thuddering in muscles, random electrical shocks going UP my leg. Going to Pain Mgmnt/Neurologist. Diagnosis lnjury to cutaneous sensory nerve, lower limb, contusion, sural and superficial peroneal neuritis, concerned with me developing CRPS. What do you believe transpired for this to have such horrible pain still after 2yrs and 2mo? Thoughts, suggestions? Thank you so much!!
Tina, this does sound like a neurological issue, but I could make any guesses. A neurologist can test individual nerves. Bone bruise alone causes only localized pain. I suggest you to insist in getting exact diagnosis and proper treatment.
Good Morning, I fell on February 12th 2016 I did not walk for 14 weeks below is my list of imaging results with my injuries. My question is I have just recently began to work out non weight baring exercises and riding a bike and I am struggling massively my leg is turning purple again when I stand and struggling to get circulation I need exercise so desperately so do I push threw and continue to exercise or do i stop and give it more time? Do I go back to the Ortho?
There is some bone marrow edema involving the lateral femoral condyle, There is mild thinning and irregularity of the posterior patellar articular cartilage 1. Large joint effusion. 2. Bone contusion in the lateral femoral condyle. 3. Grade 1 sprain of the medial collateral ligament. 4. Mild subluxation of the patella relative to the distal femur. I then 2 days later got 3 DVTs in my calf.
Tiffany, obviously that exercise is currently too much for you. Yes, I suggest you go back to an orthopedician.
I had a really bad injury to both shins and had huge “goose eggs” on front of my shins. I didn’t go to the doctor because I could walk, not without tremendous pain. It has been over 6 months and I still have bruising and pain. Is it too late to get treatment?
Angie, it’s not too late, but do not hesitate now. First you need to get an exact diagnosis – is it a bone bruise, tendon injury or something else.
I injured the ball of my foot in May 2015 . X-rays at the time showed no injury. I have RA, so my symptoms (though asymetrical) were dismissed as that originally. Unfortuantely, that meant that I did not rest the foot at all when the injury occured (the RA mentality of ‘just get on with it’ kicked in). But an MRI 6 months later revealved bone bruising of the second metatarsal head.
That was last December and almost a year later I still suffer with daily pain (ranging between a niggle and not being able to put weight on it at all). It feels like a bruise in that it only hurts when pressure is applied (which makes me think that the pain is releated to the original injury rather than the RA). So I was interested to read that a bone bruise can take up to 2 years to fully heal. But my question now is: could having RA be preventing the inury from healing?
Vickie M, I don’t know how much of impact RA could have on a bone bruise. RA occurs in the joint while the bruise is in the bone. I think the more important question is if there is any stress fracture (“hairline” fracture) in the bone, which could be a source of continuous bleeding. A doctor can say if an additional MRI could reveal anything important.
Thanks, Jan. I’m sure you’re right. Interesting article! I’ll probably bring it up during my next meeting with the doc.
I have been diagnosed with a Bone contusion to the medial condial of my femur after “microfracture” surgery. I am 5 months post-op. The cartilage repair seems to be working well,but I am unable to walk more than 15 minutes without pain. I followed post-op weight bearing restriction exactly as directed by my doctor and PT. Have you seen this type of complication before after “microfracture” and do you have any further suggestions for recovery? Thanks.
Heather, I am not a doctor, so I do not have experience with this. The surgeon who operated you or some other surgeon who knows this can comment if this healing time is normal and if not what could be the problem. Maybe a microfracture did not heal well and is a continuous source of blood in the bone.
Hello Jan, I am curious to know if you could suggest any treatments, whether home or via the doctor, to reduce rather extreme swelling in my knee due to a “significant bruise” to my tibia about 2.5 months ago. I have been on resting, keeping the joint wrapped at all times, icing, elevating since the injury and have been on crutches for about 3 weeks now following the diagnosis. I am pain free and have good range of motion by now, but I still have a knee about the size of a softball. I suggested “sucking out the fluid” to the doc and he was quite obviously unimpressed with that idea. Do you have any other ideas about treatment I could ask about at the follow up appointment? Or anything else i can do at home? For reference I am in my 20s and otherwise healthy and very active when both legs are cooperative. Thank you!
Hi Meg,
I came across this site having just been diagnosed via MRI with”significant bruising” on three of my ankle/foot bones from a fall in October. I am glad you are on the road to recovery – I have just started!
I would like to suggest something more herbal or homeopathic to help with your swelling. Obviously you would want to be prudent and choose an option that you are comfortable with, but you might find it effective. For example, I have a long relationship with using yarrow (Achillea millefolium) both internally and externally for fevers and fluid reduction. There are a lot of options in potentially effective plants and in how they are administered (ranging from store bought infusions to at home whole plant preparation).
I will let you do your own searching if you have interest, but I am a science teacher and can vouch that traditional medicine (I usually do my own preparation) does have a place even alongside more western white coat medical practices. Good luck!
Another thought: if herbs are a little too non-mainstream, Epsom salts are also a good idea. My doc swears by them and has had me soaking my ankle every night. (A hot water solution helps me.) You could probably do a compress for your knee since it’s a little more difficult to soak the middle of your leg than the end 🙂
Hi Jan,
What an awesome forum for those of us with bone bruise questions…and thanks for taking the time to answer them! 🙂
I suffered a complete ACL tear, high grade/possible complete MCL tear, partial tear of proximal fibular collateral ligament & questionable tear of lateral meniscus with bone contusions in the lateral femoral condyle & lateral tibial metaphysis back in early June. The orthopedic surgeon I finally saw in August felt I had sufficient stability & surgery was not required, just a brace & physiotherapy. I saw him again in late September & his comment was the ACL was healed but the bone bruise was now the biggest issue. He did say this could take upwards of 8 months to heal. I have recently been given the green light to begin running again but am thinking I may be aggravating the bone bruise & thus prolonging it’s healing with such impact. What is your opinion?
I would like to be able to compete in the World Masters Games in April 2017 but the surgeon says my chances are only 50/50 at this point. 🙁
Denise, it seems your surgeon is giving you a realistic advice about “8 months” — meaning to avoid any unnecessary strain to the leg in this period. My personal opinion is: do what your inner voice is saying to you – do you feel peace in your heart to go running in April 2017 or not? It’s a yes or no answer. No cheating.
I sprained my left ankle in mid May, within 24 hours foot started turning purple and swelling, quite similar to CRPS, which I experienced in my right arm in 2008. Foot turned green, yellow and all bruising disappeared in about a month. X-rays of foot and ankle negative. I continued to have symptoms of CRPS (on/off swelling, extreme pain, tingling, muscle twitching, extreme cold etc). Finally had MRI mId August, diagnosed 3 bone contusions. Could I have both bone bruise and CRPS? I used crutches for about 6 weeks, foot still hurts quite a bit and most of CRPS symptoms remain. Thank you…
Susan, bone bruise causes pain and is obviously associated by skin bruising. Bone bruise by itself should not cause temperature changes, muscle twitching and tingling, so you may want visit a neurologist.
Just diagnosed with talus bone marrow edema from recent MRI and instructed on complete non weight bearing of the foot. Initial injury was 4 months ago with hyperextension inversion injury, wore a boot for 5 weeks after injury. How dangerous is this injury and would it be ok to do a 70 mile bike ride in 2 months.
Renee, bone marrow edema heals slowly, so I personally would avoid any extra physical activity for some time (probably 1 year from initial injury). But the doctor should know better.
I hit my ankle one week ago, there was an immediate large haematoma due probably to chlopydegrol and aspirin intake. It is now 10 days later still in a lot of pain and whole foot is swollen. Icing up to 5 times a day the foot cannot bear to be warm
Val, you may want to check this with a doctor, who might suggest an X-ray to see if any bone is broken.
I fell on 6/9/16 and injured my R hip and suffered a small labrum tear along with the MRI noting a bruise in the hip area. I also suffered a tibia plateau fx just below the kneecap on my L leg. I am in my late sixties and have an appt to see an Ortho. I was out of State at the time and saw my family MD on 6/24. Can you suggest specific questions I should ask the Ortho about the hip bruise? At the time the ER MD told me to keep active not knowing I had fx’d my L leg so I had been walking on both injuries since 6/9!!!!
Mary Helen, by keeping active the doctor probably meant not to rest in bed, but maybe not walking around too much.
You may want to ask the orthopedist:
– What is the exact name of the damage in the femoral head and hip joint (“bone bruise,” “hair fracture” “bone marrow edema” “labrum tear,” etc.)? Write down the answer or ask for a copy of a document with the exact diagnosis.
– In what time you can expect full recovery? Do not be surprised if it will be “one year.”
– How active should you be: to walk or not, to have some exercises or not…?
– Medications to take or avoid?
Note that when the pain goes awaythis does not already mean that the bone bruise has healed completely (this can be evaluated by another MRI, if necessary).
Going on almost a year of severe pain after a slip and fall. The MRI shows edema of the bone marrow of the 4th metatarsal. I have had steroid injections, iced, immobilized, cold laser therapy but nothing seems to work. I have been to many doctors but none have been able to give any sort of care plan. Has anyone found something has worked? Getting desperate for something to work.
Joe, this is quite specific question. You may want to join some of health forums to get more ideas.
My 76 year-old mother was diagnosed with a “very large and bad bone bruise” of the left knee, along with an ACL tear and tears in her meniscus. She had a scope but continued to have significant pain and swelling. Four weeks after her scope (right and left side of her meniscus were removed) we took her back in due to ongoing pain and swelling. The MRI showed avascular necrosis with collapse of her bone on the outside of her left knee. She will have a total knee replacement tomorrow. Could the avascular necrosis be a direct result of her bone bruising? After the knee replacement, is there any possibility the bone could continue to die? Thank-you for taking the time to answer my questions.
Columbusgal, it is possible that avascular necrosis is a direct result of bone bruise, but they both have developed as a result of an injury if I imagine this right. Avascular necrosis can also develop after an injury without a bone bruise. If the damaged bone will be removed and replaced, I see no reason why would her knee bone continue to die — assuming that surgery will go well and her bones are otherwise healthy.
After a bad fall I had an MRI. No fracture on xrsys) Rheumatologist using ultrasound diagnosed wrist haemarthrosis. He said MRI showed evidence of bone bruising. After 6 wks I expected more healing. Large lump still on back of my hand, expected further 6 wks to heal. Tendons in my wrist ‘snap’ painfully. wrist still aching. Will there be lasting damage?
Donna, bone bruise may need several months to heal. The lump you’ve describe is not from bone bruise but from the swelling of the joints in the wrist. You may want to ask a doctor if a steroid injection would help. It is possible that your wrist will heal completely, but you probably need to give it more time.
What would the reason be to send someone to get blood work done after an MRI showed a bone bruise on the knee? Was informed they were worried about the large size of the bruise and there was a patchy area. There was no further elaboration on the reason for the blood test.
Kaityn, they could check for an eventual blood clotting disorder, which could be the reason for the large bruise size. Another reason is to rule out bone cancer or some other disorder.
Do you have any additional info on #37. I had an MRI and was told I have a bone bruise. I am in a lot of pain and they want to immobilize it for four to six weeks 24/7 …. at least as much as possible with a brace.
It has been a year with this pain and it seems a long time for what they term a “bruise”. Any additional information would be appreciated.
Kristi, what additional info (#37 ?)? A bone bruise can actually last as long as you mentioned. I which exact bone do you have a bruise and how it happened?
Hell0, How do I find your references? In particular, what is reference #6?
Regards
Michael, scroll down to the bottom of the article and click on References
The ref #6 is
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3445054/