What is pneumonia and what does cause it?
Pneumonia is an inflammation of the lungs caused by bacteria, viruses or fungi [1]. Infants, individuals older than 65 years and those with chronic diseases or impaired immunity are at greatest risk.
Pneumonia can be mild or severe. Properly treated pneumonia in otherwise healthy individuals has an excellent prognosis, but if untreated, especially in those with impaired immunity, it can be life-threatening. Pneumonia is a major cause of death all over the world [24].
Word origin (etymology) of pneumonia: from the Greek pneúmon = lung [2]
- American (US): noo-mohn-yuh
- British (UK): nju-mohn-ia
Medical abbreviation of pneumonia: PN or PNA [3]
Pneumonitis is a group of diseases with lung inflammation without infection.
Chart 1. Pneumonia Facts |
|||
Bacterial |
Viral |
Atypical (Walking) |
|
| Causes | Streptococcus pneumoniae, Haemophilus influenzae… | Influenza virus, RSV… | Mycoplasma, Legionella, Chlamydophila… |
| Incubation period |
|
|
|
| Symptoms |
|
|
|
| Auscultation by the stethoscope |
|
|
|
| Duration |
|
|
|
| Spread |
|
|
|
| Who gets it |
|
|
|
| Diagnosis |
|
|
|
| Treatment |
|
|
|
| Prevention |
|
|
|
Pathophysiology – How does pneumonia develop?
Microbes can reach the lungs by inhalation, aspiration (the entrance of solid or liquid material into the lungs, for example, during vomiting) or by blood, for example, in intravenous drug users or during blood infection or septicemia (septic pneumonia).
Microbes activate the immune cells (leukocytes, macrophages) in the lungs, which results in inflammation and fluid and pus accumulation in the air sacs (alveoli). Sometimes, inflammation occurs only in the spaces between the air sacs (interstitial space) without fluid accumulation within the air sacs.
Pneumonia Types
A. By Setting
- Community-acquired pneumonia (CAP) occurs outside healthcare institutions.
- Institutional-acquired pneumonia (IAP)
- Hospital-acquired pneumonia (HAP) or nosocomial pneumonia (NP)
- Intensive care unit (ICU) pneumonia
- Healthcare-associated pneumonia (HCAP) is the one that develops in the outpatient setting or within 48 hours of admission to a hospital. It includes nursing home-acquired pneumonia (NHAP).
- Ventilator-associated pneumonia (VAP) develops from machines that assist in breathing if it develops more than 48 hours after endotracheal intubation or within 48 hours of intubation removal.
B. By Cause
- Bacterial pneumonia
- Viral pneumonia
- Atypical pneumonia: walking (mycoplasmal) pneumonia, Legionnaires’ disease
- Fungal pneumonia
- Zoonotic pneumonia
C. By Course
- Acute
- Fulminant, galloping
- Chronic
- Residual
- Recurring
- Relapsing
- Antibiotic resistant
D. By the Location/Pattern of the Lung Involvement
- Lobar pneumonia affects one or more lung lobes, for example:
- Left lower lobe (LLL), right middle lobe (RML)
- Multilobar (more than one lobe), panlobar (all lobes)
- Bronchial pneumonia (bronchopneumonia, multifocal or lobular pneumonia)
- Single pneumonia affects one lung wing and double pneumonia both lung wings; triple pneumonia is pneumonia in both lungs that was already cured, but it recurred
- Perihilar pneumonia affects the part of a lung around the hilus
- Basilar pneumonia affects the bottom parts of the lung.
- Bronchiolitis obliterans organizing pneumonia (BOOP) or cryptogenic organizing pneumonia
- Focal organizing pneumonia
- Disseminated focal pneumonia
- Alveolar pneumonia
E. By the Tissue/Cells Involved
- Eosinophilic pneumonia
- Interstitial:
- Usual interstitial pneumonia (UIP)
- Nonspecific interstitial pneumonia (nsip)
- Desquamative, nonspecific or lymphoid pneumonia
- Cavitary pneumonia
- Necrotic or necrotizing pneumonia
- Nodular pneumonia
- Giant cell pneumonia (after measles; rare, deadly)
Other Types of Pneumonia
- Aspiration pneumonia after aspiration of a solid or liquid material
- Chemical pneumonia can be caused by inhalation of irritating chemicals
- Eosinophilic pneumonia, which is not true pneumonia, because it is not an infection, but possibly an allergic reaction
- Secondary pneumonia is a term for pneumonia that develops as a complication of some other disease, for example, post-viral pneumonia in a patient with the flu.
- Opportunistic pneumonia is pneumonia that develops in individuals with impaired immunity, for example, due to treatment with steroids or chemotherapy, cancer or sickle cell anemia. Pneumocystis pneumonia (PCP) typically occurs in individuals with HIV/AIDS.
- Hypostatic pneumonia can occur due to infection in less ventilated parts of lungs, mainly in older bedridden individuals.
Diagnosis
A doctor can make a diagnosis of pneumonia on the basis of your medical history, physical examination and investigations.
Physical examination:
- Tapping parts of the chest (percussion) can provoke dull sounds.
- Listening to the lungs by the stethoscope (auscultation) can reveal crackling sounds and decreased breath sounds.
Investigations:
- Sputum (coughed up mucus) culture
- Blood tests:
- Blood culture
- Immunoglobulins against viruses
- Complete blood count (CBC)
- Pleural fluid culture
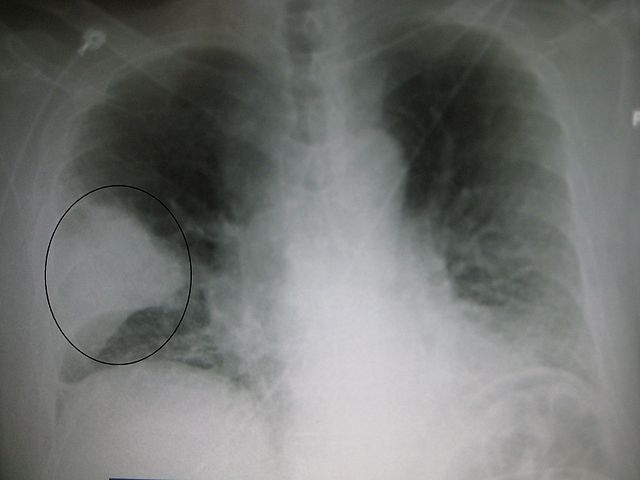
- X-ray: The diagnosis of pneumonia can be made only if white shadows are present on the film.
- Pulse oximetry–a quick test to measure oxygen in the blood
- Arterial oxygen saturation
- Bronchoscopy can be done to detect eventual obstruction in the bronchi.
- Computer tomography (CT) can reveal pleural effusion or pneumonitis.
- Ultrasound can detect lung abscess.
- Pneumonia severity index (PSI) or PORT score
- References: [4,5]
Picture 1. The white shadow on an X-ray film (within the circle)
suggests pneumonia in the middle lobe of the right lung.
(source: Wikipedia, Creative Commons license)
Treatment
Early treatment usually results in faster recovery and fewer complications.
Bacterial pneumonia [6]:
- At home: bed rest, enough fluid, oral antibiotics, painkillers (ibuprofen) [10]
- In hospital: intravenous antibiotics, oxygen by mask [18] or in severe cases, mechanical ventilation that may require intubation or tracheostomy [8] NOTE: The insertion of breathing tube for mechanical ventilation by itself increases the risk of bacterial pneumonia [22].
- Antibiotic-resistant bacteria, which are resistant to common antibiotics, should be treated with alternative antibiotics:
- Klebsiela pneumoniae that produces carbapemenase (KPC): gentamicin, tigecycline, and colistin [23]
- Methicillin-resistant Staphylococcus aureus (MRSA): vancomycin or trimethoprim- sulfamethoxazole [8].
Viral pneumonia usually does not require any special treatment and it can heal on its own. If started early, antivirals (acyclovir, cidofovir, oseltamivir, palivizumab, ribavarin or zanamivir) may shorten the duration of pneumonia in some cases.
Fungal pneumonia can be treated by antifungals (itraconazole, amphotericin B).
Atypical pneumonia caused by Mycoplasma, Legionella or Chlamydophila can be treated with antibiotics (azithromycin, clarithromycin, erythromycin, doxycycline).
Other drugs, if prescribed:
- Centrally acting anti-cough medicines may prevent you coughing up mucus properly, so speak with a doctor about using them.
- Steroids. There is weak evidence about beneficial effects of corticosteroids in the treatment of pneumonia [12,13,14].
Exercises:
- Make a deep breath, hold it for a while, then cough up mucus and spit it out. Repeat 10 times every hour during the day [10].
- Tap your chest few times a day while lying with your head lower than your chest — this may help remove some mucus from your lungs [21].
There is insufficient evidence about the beneficial effects of vitamin C [15], essential oils [20], over-the-counter (OTC) cough medicines [19] and chest physiotherapy in children [16] or adults [17] in preventing or treating pneumonia.
Recovery Time/Prognosis
In otherwise healthy individuals, pneumonia, when treated properly, is usually a benign disease, which can last for few weeks and heal completely without complications [1]. Untreated atypical pneumonia can last for several months.
In infants, elderly and individuals with chronic diseases, pneumonia can be a serious illness, which can be deadly if not treated promptly.
Complications
Complications of pneumonia more likely occur in young infants, elderly and in individuals with diabetes, impaired immunity (HIV/AIDS) or liver cirrhosis (alcoholics) [4].
- Pleurisy — inflammation of the lung membrane
- Pleural effusion — fluid accumulation between the lung membranes–, which may get infected (empyema)
- Inability to breath in enough oxygen (respiratory failure); requires breathing machine or ventilator
- Acute respiratory distress syndrome (ARDS)
- A pus-filled cavity in the lungs (lung abscess)
- Spread of infection to the blood (septicemia) and other organs (sepsis)
- Atelectasis — collapse of a lung lobe
- Pneumothorax — collapse of a lung wing
- References
- Pneumonia Encyclopaedia Britannica
- Pneumonia Dictionary.reference.com
- Medical abbreviations GlobalRPh
- Pneumonia Johns Hopkins Medicine
- Amanullah S, Typical bacterial pneumonia imaging Emedicine
- Kamangar N, Bacterial pneumonia Emedicine
- Pneumococcal disease, clinical features Centers of Disease Control and Prevention
- Kamangar N, Bacterial pneumonia, treatment Emedicine
- Mosenifar Z, Viral Pneumonia, overview Emedicine
- Viral pneumonia Drugs.com
- Mycoplasma pneumoniae infection causes and transmission Centers of Disease Control and Prevention
- Chen Y et al, 2011, Corticosteroids for pneumonia Cochrane
- WAn JD et al, 2016, Efficacy and Safety of Corticosteroids for Community-Acquired Pneumonia: A Systematic Review and Meta-Analysis PubMed
- Salluh JIF et al, 2008, The role of corticosteroids in severe community-acquired pneumonia: a systematic review PubMed Central
- Hemilä H et al, 2013, Vitamin C for preventing and treating pneumonia Cochrane
- Chaves GSS et al, 2013, Chest physiotherapy for pneumonia in children Cochrane
- Yang M et al, 2013, Chest physiotherapy for pneumonia in adults Cochrane
- Zhang Y et al, 2012, The effectiveness of oxygen for adult patients with pneumonia Cochrane
- Chang CC et al, 2014, Over-the-counter medications to help reduce cough for children and adults on antibiotics for acute pneumonia Cochrane
- Naveed R et al, 2013, Antimicrobial activity of the bioactive components of essential oils from Pakistani spices against Salmonella and other multi-drug resistant bacteria PubMed Central
- Pneumonia – adults (community acquired) MedlinePlus
- What Are the Risks of Being on a Ventilator? National Heart, Lung and Blood Institute
- Qureshi S, Klebsiella Infections Treatment & Management Emedicine
- Chow S, Pneumonia Epidemiology News-Medical