Myofascial Pain Syndrome Definition
Myofascial pain syndrome is a chronic regional musculoskeletal pain disorder with trigger points in the muscles and referred pain in distant body parts (1). For example, applying pressure to the shoulder blade muscles can trigger pain in an arm. The pain supposedly arises from the fascia — a thin sheath of connective tissue wrapped around the muscles.
Synonyms: myofascial pain syndrome (MPS), chronic myofascial pain (CMP), myofascitis
NOTE: The information in this article bases on a limited number of studies. According to some authors, there is insufficient scientific evidence about the existence of trigger points and effectiveness of current treating techniques (21).
Causes and Risk Factors
- Repetitive muscle overload or injuries in sports, such as golf, weight lifting or running, or due to carrying heavy bags, playing an instrument, such as violin, piano or drums, or due to obesity, pregnancy or breastfeeding
- Poor posture (rounded shoulders) during prolonged sitting (study, computer work) or standing in combination with lack of exercise
- Psychological stress, such as anxiety or depression
- Acute muscle injury: contusion or strain
- Osteoarthritis, rheumatoid arthritis, systemic lupus erythematosus (SLE) (19)
- Nerve root compression due to bulging or herniated disc in the spine
- Visceral pain: inflammation of the internal organs (appendix, gallbladder, stomach), angina pectoris (in ischemic heart disease), kidney stones
- Lifestyle issues: lack of sleep, smoking
- Cold weather or sleeping in front of air condition
- Hormone imbalance: hypothyroidism, hyperuricemia, hypoglycemia or estrogen deficiency after menopause
- Nutritional deficiencies: iron deficiency anemia or low blood levels of calcium, potassium or vitamins B1, B6, B12, C or D
- Leg length discrepancy
- Scoliosis (sideways curvature of the spine)
- Connective tissue diseases, such as Marfan and or Ehlers-Danlos syndrome
- References: (1,3,6,20,24)
Myofascial pain can appear at any age and affects men and women equally (20).
Symptoms and Signs
Muscle Knots
One or more muscle knots–tender nodules–and taut bands–rope-like indurations under the skin, also called myofascial adhesions or “muscle guarding” (reflex spasm)–can be detected with the fingers in various parts of the body (see below) (1).
Myofascial Pain and Trigger Points
The pain is usually limited to one body region, for example, upper or lower back, is deep and dull, mild or shooting, burning, throbbing or cramp-like and can have a sudden or gradual onset. It can be constant or waxing and waning and present at rest or only during activity (1).
Trigger point characteristics:
- Snap, pinch or pressure upon the muscle knots triggers muscle twitches at the site of the snap
- Continuous pressure lasting more than 5 seconds (19) triggers pain and abnormal sensations (paresthesia), such as tingling, pins and needles, coolness or excessive sweating in distant body parts (referred pain) and a “jump sign”–a movement of the body part “away” from the pain (1).
- The pain threshold in the skin overlying the muscle knots can be decreased, while in other skin areas it remains normal (1). Except for lowered pain threshold, skin sensations during the examination are normal (3).
Trigger point types:
- Active trigger points are painful upon pressure.
- Latent trigger points are not painful upon pressure; they can eventually develop into active trigger points.
- Reference: (1)
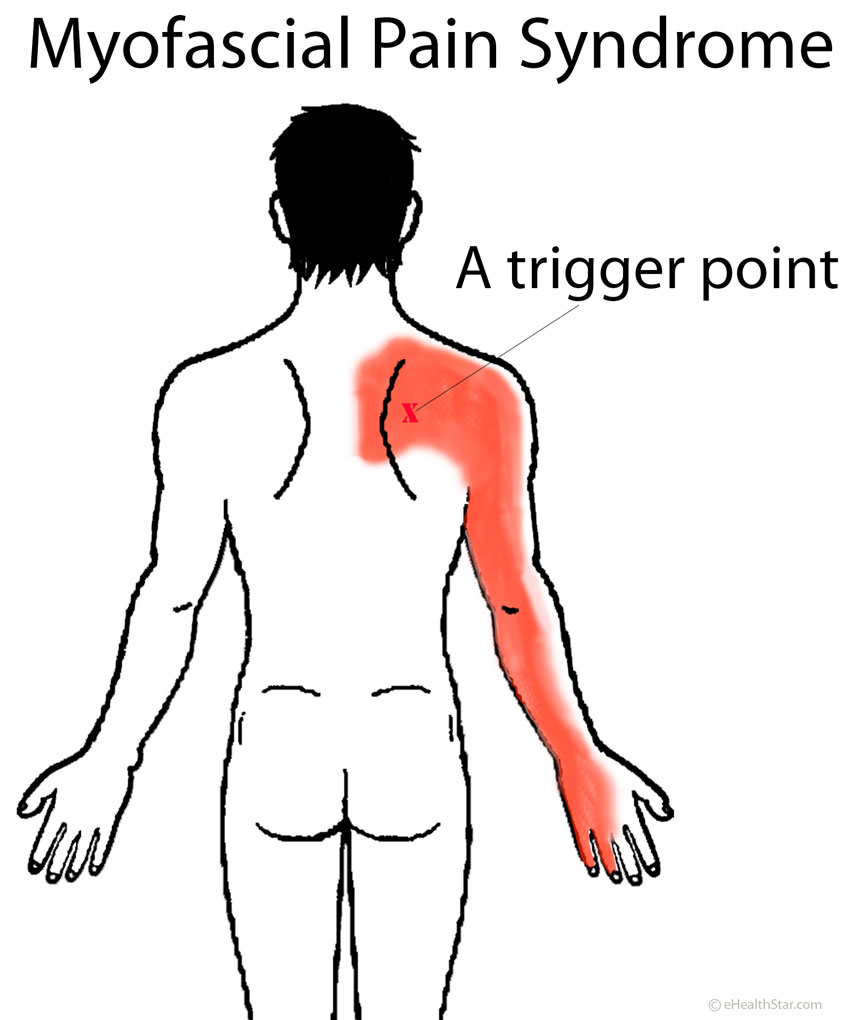
Picture 1. Myofascial pain arising from the shoulder blade area:
Pressure on a trigger point can cause pain over the shoulder blade and down the arm.
Other Symptoms
- Muscle stiffness, fatigue, weakness (but no significant muscle wasting), incoordination, restriction of mobility (decreased range of motion) in related joints can appear.
- The syndrome can be associated with a headache, migraine, poor memory, insomnia, temporomandibular joint dysfunction or fibromyalgia.
- Reference: (1)
Trigger Points Locations
For detailed locations of trigger points all over the body–from the head to the feet–check this symptoms checker.
Neck and Head
- Trigger points in the neck can often be identified in persons with a migraine, tension headache or a headache after an injury, such as whiplash injury, and in those with temporomandibular joint dysfunction, toothache and sinus pain (1).
- Symptoms can include pain and tingling in the neck that radiate to the arms, headache, dizziness, nausea, insomnia, excessive tearing and sweating, tinnitus, drooping eyelid (ptosis) on one side of the face, dizziness and impaired balance.
- Signs:
- Decreased range of motion in the neck
- Lumps (knots) and trigger points in the muscles: trapezius, rhomboid, sternocleidomastoid, supraspinatus, infraspinatus and levator scapulae
- Differential diagnosis: wry neck or torticollis, neck sprain, fibromyalgia, degenerative disc disease, spondylitis, thoracic outlet syndrome
- Reference (4)
Shoulders – Rotator Cuff
- Dry needling may be an effective treatment for myofascial pain in rotator cuff muscles but more research is warranted.
Upper Back – Trapezius Strain
Trapezius strain is characterized by discomfort, tightness and muscle knots between the shoulder blades. Pain and tingling can radiate to the shoulders, neck and head. Causes include poor posture, repetitive lifting, workout exercises, such as pull-ups, tilting the head sideways when using the phone, scoliosis and leg length discrepancy (2).
Lower Back – Myofascial Lumbar Strain
- Muscles along the spine in the lower back are most commonly affected (10).
- Disorders of the joints between the lumbar vertebra (facet joints) can cause myofascial pain in the lower back (11).
- One possible cause of myofascial lumbar sprain is repetitive pain from kidney stones, which may result in trigger points in the lower back. Pressure on these points may trigger pain similar to one caused by kidney stones (1).
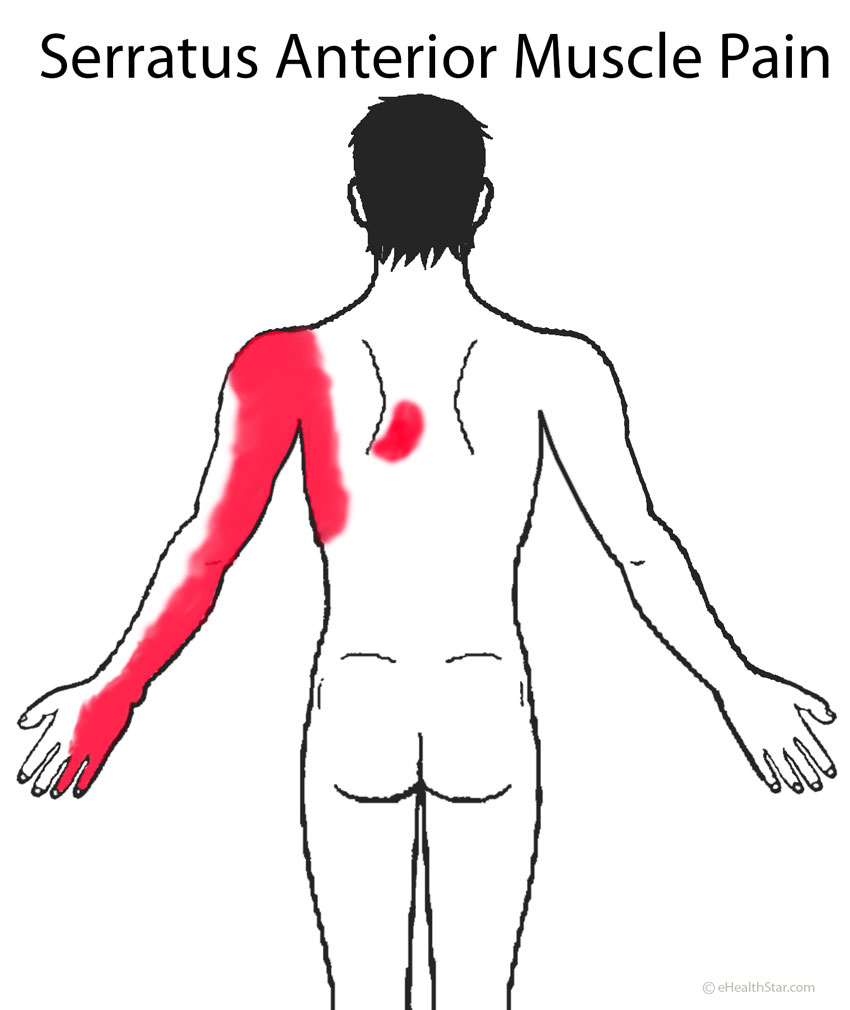
Chest – Serratus Anterior Muscle Pain Syndrome
Serratus anterior muscles on both sides of your chest, below the armpits, help raise your upper arms forward and upward, for example, during sprint, workout exercises (push-ups, bench presses) and expand your chest during breathing in. Repeated sprints, prolonged running or prolonged hard coughing can cause pain between and below the shoulder blades and on the inner sides of the arms down to the pinky and ring finger (Picture 2); the pain can be aggravated by deep breathing.
Picture 2. Serratus anterior muscle pain distribution:
on the side of the chest, below the shoulder blade
and down the inner side of the arm
Buttocks – Piriformis Syndrome
The piriformis muscle originates at the lumbar spine in the lower back and ends on the top of the femur (upper leg bone) on each side. The irritation of the muscle due to repeated prolonged running or fall on the buttock, can cause muscle knots and swelling in the muscle and compression of the sciatic nerve (17).
Pain can appear in the buttock, hip, coccyx or groin and can radiate down the back of the thigh, into the calf or foot, usually only on one side. The pain resembles sciatica ) sciatica (pain in the lower buttocks that radiates down the back of the thigh (10).
Applying pressure on trigger points in the buttock muscle can trigger pain mimicking sciatic pain (19).
Myofascial Pelvic Pain (MFPP) in Women
- Trigger points are in the pelvic floor muscles (around the anus and vagina). Pain may radiate to the lower back, abdomen or thighs.
- Causes and risk factors: birth trauma, chronic poor posture, repetitive movement patterns, joint hypermobility, leg length discrepancy, scoliosis, pelvic torsion, surgery, childhood falls, physical or sexual abuse
- MFPP may be caused or it may result in urinary urgency or frequency (overactive bladder), irritable bowel syndrome (IBS), interstitial cystitis/painful bladder syndrome, urge incontinence, constipation, painful intercourse (dyspareunia), endometriosis, pain in the vulva (vulvodynia), coccyx pain or pudendal neuralgia.
- Pain may be also triggered by menstruation, prolonged sitting or walking, bowel movements or intercourse.
- Reference: (24)
Thighs – IT Band Syndrome
Iliotibial (IT) band is a band of fascia that runs from the hip over the muscles on the front side of the thigh and ends below the knee. Overstretching of the IT band can cause stinging pain, swelling or underskin thickening on the outer side or above the knee or along the entire length of the IT band.
Main causes include repetitive running, hiking, cycling, rowing and weight lifting.
Calf
Trigger points in the gastrocnemius muscle in the calf can cause calf cramps at night (27).
Feet – Plantar Fasciitis
Pain in the soles of the feet in plantar fasciitis is technically not myofascial pain since it does not arise from muscle fascia but from a thick sheet of connective tissue called plantar fascia. Causes of plantar fasciitis include prolonged walking, running or standing. The main symptom is the pain in one or both soles in the morning, which improves with walking. The pain can be prevented by feet massage before first steps in the morning.
Video 1. Myofascial syndrome: Trigger points
Diagnosis
A doctor can usually make a diagnosis of myofascial pain by physical examination. Electromyography (EMG) can detect muscle fatigue, ultrasound can detect local twitch response and thermographic examination may detect hot spots.
Myofascial pain can resemble fibromyalgia. The two conditions can also appear together.
Chart 1. Myofascial Pain vs Fibromyalgia |
||
| Myofascial Pain | Fibromyalgia | |
| Pain characteristics | Trigger points — pressure causes pain in the trigger point and in a distant area | Tender points — pressure causes pain only in the tender point |
| Pain distribution | Localized, non-symmetrical | Generalized, symmetrical |
| Jump sign | Yes | No |
| Fatigue | Sometimes | Usually |
Other conditions that can mimic myofascial pain:
- Chronic fatigue syndrome (CFS): persistent, profound fatigue not relieved by rest, various vague pains
- Muscle strain: localized pain, tenderness and swelling
- Tendonitis or tendinitis: pain near the joints (elbow, knee, above the heel) aggravated by movements, tenderness to touch, swelling
- Neuropathy: pain, numbness and tingling in feet and hands in a “stockings and gloves pattern;” causes include diabetes, alcoholism, vitamin deficiencies, injury
- Referred pain in heart, gallbladder, pancreatic disorders; the pain radiates into the left or right shoulder or between shoulder blades
- Complex regional pain syndrome (CRPS): burning pain and hypersensitivity to temperature, usually in a limb
- Central pain syndrome includes burning pain, tingling and hypersensitivity to touch and temperature; it can occur after spinal cord injury or in neurological disorders, such as multiple sclerosis, Parkinson’s disease or stroke.
- Polymyositis and dermatomyositis: symmetrical muscle weakness in the limbs, skin rash (usually after age of 45)
- Polymyalgia rheumatica: symmetrical stiffness in the pectoral girdle muscles and around the hips (usually after age of 65)
Conditions that can mimic muscle knots:
- Rheumatoid nodules
- Ganglion cyst, for example, in the wrist, finger, behind the knee or on top of the foot; may be painful or not
- Enlarged lymph nodes in the back of the head, in the front of the neck, in the armpits, groin or behind the knee (in lymphoma or metastatic cancer)
- Contracture deformity: replacement of elastic with nonelastic tissue in the skin or muscles due to injury, burns, nerve damage or prolong immobilization
- Neurofibromatosis
- Nodules in infections, such as tuberculosis, leprosy, syphilis and leishmaniasis
Treatment of Myofascial Pain Syndrome
1. Correction of the Underlying Causes
Correction of bad posture, leg length discrepancy, sleeping habits, diet, coping with stress, decrease of intensity or frequency of exercise, other lifestyle changes and treatment of eventual chronic infections may be needed before the start of active treatment.
2. Stretching Exercises (Spray-and-Stretch)
Stretching exercises can help in early phase of myofascial pain that is limited to one body area (1).
- Spray the sore are with vapocoolant spray and stretch the muscle but only until the pain appears (1). Initially, a physiotherapist can be involved.
3. Trigger Point Pressure Release (Direct Release)
A therapists applies increasing pressures along the affected muscle with his fingers until he identifies a muscle knot and maintains pressure until the tension in the knot is released (1). During the procedure, a therapist can spray the affected area with a vapocoolant spray or inject a local anesthetic into the knot to prevent pain during the procedure.
Contraindications for trigger point release: malign tumor, aneurysm, acute rheumatoid arthritis, healing fracture, severe osteoporosis, advanced diabetes mellitus (9).
4. Self Myofascial Release Techniques (SMRT)
Roll over a foam roller or ball using your body weight. Some physiotherapists advise holding the pressure at trigger points for up to 20 seconds. The exercise can be quite painful.
SMRT Benefits
In some studies, foam rolling over the hamstring muscle for up to 10 seconds increased the range of motion (ROM) of the leg by 4.3% (12), and rolling over the quadriceps muscle for 2 minutes increased ROM in the knee for 10 degrees (13).
In one study in individuals with neck and lower back pain, using foam roller for up to 12 minutes was associated with decreased pain (14). Myofascial release can also reduce pain in tennis elbow (epicondylitis) (15).
Compression Tools for Myofascial Pain
- A foam roller
- A tennis ball or Lacrosse ball
- A rounded stick
5. Trigger Point Injection and Dry Needling
According to several studies, an injection of a local anesthetic, such as lidocaine, can inactivate trigger points (1,6). The conclusion of one 2009 systematic review of studies was that there is insufficient evidence about the effectiveness of dry needling in myofascial pain relief (34).
In one study, needle electrical intramuscular stimulation (NEIMS) of shoulder had positive effects on cervical myofascial syndrome (7).
Side effects and risks of injections and dry needling may include bleeding, hematoma, pain, fainting, infection and lung puncture (pneumothorax) (11,32).
Contraindications. Individuals taking aspirin or other anticoagulants and those with bleeding disorders, local or systemic infections, allergy to anesthetics or acute muscle injury should not get muscle knot injections or dry needling (33).
6. Home Remedies
- Ice packs for 20 minutes, when applied within 72 hours after an injury can reduce inflammation and pain (6).
- Heat pads, hot showers or whirlpool massage can be effective after the third day after the injury (4,6).
- Appropriate chair and mattress can help prevent the pain recurrence.
7. Muscle Strengthening
After the myofascial pain is relieved, exercise to improve the strength of the affected muscles can help prevent recurrence of the pain (19).
8. Other Possibly Effective Treatment of Myofascial Pain
- Lidocain or diclofenac sodium patch
- Transcutaneous electrical nerve stimulation
9. Insufficient Evidence
There is insufficient evidence about the effectiveness of the following methods in relieving myofascial pain (1,5,6):
- Classical mechanical massage (8)
- Chiropractic manipulation
- Rolfing structural integration (a type of soft tissue mobilization by aligning and balancing the body with gravity)
- Cupping or myofascial decompression
- Fascial unwinding (a type of myofascial release in which a patient moves the body part to areas of ease in response to the therapist’s touch) (16)
- Acupuncture (22)
- Shiatsu (ischemic acupressure) (6)
- Ischemic compression
- Kinesis myofascial integration (KMI) (25)
- Botulinum toxin injections (23)
- Therapeutic ultrasound
- Cold laser therapy (low level light therapy) (8)
- Topical analgesics: capsaicin, eucaliptus oil, menthol, peppermint and other herbal preparations
- Oral drugs or supplements: tricyclic antidepressants, gabapentin (an anticonvulsant), glucosamine, methylsulfonylmethane, copper, zinc, vitamin C, vitamin E
10. Little or No Help
- Immobilization of any kind (cervical collars, slings, braces) can worsen muscle weakness, so it should be avoided (2,28).
- Nonsteroidal anti-inflammatory drugs, such as aspirin, diclofenac, ibuprofen, indomethacin, ketoprofen or naproxen, when used alone are of only little help (1,5,6).
- Prolotherapy–injection of irritating substances, such as sucrose, in order to trigger tissue repairing process
- Steroid injections (19)
- Muscle relaxants do not help, since myofascial pain is not caused by muscle spasms (1).
- Reflexology–applying pressure on certain spots on the feet and hands
Myofascial pain syndrome is not an indication for surgery (26).
Prognosis
Myofascial pain can be cured successfully by a lifestyle change and physiotherapy, but recurrence is common (3). When myofascial pain is not managed appropriately, it can develop into fibromyalgia (19).
When there is no pain relief after 8 weeks of treatment, it is necessary to search for underlying conditions, either physical or psychological (25).
- References
- Giamberardino MA et al, 2011, Myofascial pain syndromes and their evaluation ResearchGate
- Trapezius strain Inkling
- Cervical Myofascial Pain Overview Emedicine
- Cervical Myofascial Pain Clinical Presentation Emedicine
- Cervical Myofascial Pain Medication Emedicine
- Chandola HC et al, 2009, Fibromyalgia and Myofascial Pain Syndrome-A Dilemma PubMed Central
- Lee SH et al, 2008, Effects of needle electrical intramuscular stimulation on shoulder and cervical myofascial pain syndrome and microcirculation PubMed
- Jafri MS, 2014, Mechanism of myofascial pain Hindawi
- Myofascial release (MFR): an overview Hospital For Special Surgery
- Chen CK et al, 2011, Myofascial Pain Syndrome in Chronic Back Pain Patients CiteSeerX
- Huang JT et al, 2014, Lumbar facet injection for the treatment of chronic piriformis myofascial pain syndrome: 52 case studies PubMed Central
- Sullivan KM et al, 2013, ROLLER MASSAGER APPLICATION TO THE HAMSTRINGS INCREASES SIT AND REACH RANGE OF MOTION WITHIN FIVE TO TEN SECONDS WITHOUT PERFORMANCE IMPAIRMENTS PubMed Central
- MacDonald GZ et al, 2013, An acute bout of self-myofascial release increases range of motion without a subsequent decrease in muscle activation or force PubMed
- Tozzi P et al, 2011, Fascial release effects on patients with non-specific cervical or lumbar pain PubMed
- 2014, Conservative care options for work-related epicondylosis National Guidelines Clearinghouse
- Minasny B, 2009, Understanding the Process of Fascial Unwinding PubMed Central
- Piriformis syndrome overview Emedicine
- Sucher BM, 1993, Myofascial release of carpal tunnel syndrome The Journal of the American Osteopathic Association
- Bennet R, Understanding myofascial pain Myalgia.com
- Physical medicine and rehabilitation for myofascial pain Emedicine
- Quintner JL et al, 2015, A critical evaluation of the trigger point phenomenon PubMed
- Furlan AD et al, 2005, Acupuncture and dry-needling for low back pain PubMed
- Cervical Myofascial Pain Treatment Emedicine
- Pastore EA et al, Recognizing Myofascial Pelvic Pain in the Female Patient with Chronic Pelvic Pain PubMed Central
- Unaproved Medical Procedures and Treatment Montana.gov
- Myofascial pain Virginia Spine Institute
- Prateepavanich P et al, 1999, The relationship between myofascial trigger points of gastrocnemius muscle and nocturnal calf cramps PubMed
- Myofascial pain syndrome OrthopaedicsOne
- Contracture deformity Medline Plus
- Tendonitis, clinical presentation Emedicine
- Pain: Hope through the research National Institute of Neurological Disorders and Stroke
- Triggers point pain Drugs.com
- Trigger Points: Diagnosis and Management American Family Physician
- Tough EA et al, 2009, Acupuncture and dry needling in the management of myofascial trigger point pain: a systematic review and meta-analysis of randomised controlled trials PubMed


I have myofacial pain from jaw down to collarbone, and a lump on jaw bone that comes and goes. I do have 3 cervical bulging discs c3-c4-c5 with myelopathy, have a t6 wedge fracture with Compression t7-t10 and lumbar bulging disc l4-l5-s1, and I also have a shoulder bursa, which sometimes get cortisone injection. So I’m presuming my cervical spine issues causing myofacial jaw pain, but I don’t understand the lump. The only treatment I’m receiving right now is pain relief (tramal) and diazepam for nerve & muscle pain. I’m stopping cortisone injections and the pills as they have made me put on so much weight I feel crushed inside. I’ve basically learned to handle the Spinal pain and other symptoms they cause, but this myofacial jaw pain, sometimes it makes me cry out a lot, but I’m learning that if I move my neck and have jaw open in certain positions it eases it. The pain, It’s like 5 toothaches at the same time, but in one spot, the jaw joint. Anyway, what I really need to know is, does this hard nodule/lump have anything to do with myofacial pain or my cervical spine??
If the lump appears and disappears quickly, it could be a muscle knot. The knot can develop as a reaction to repetitive pain episodes. You may want to ask a doctor to check it.
I have a very small lump on my back of my neck, it is near my right side hairline. It cannot be seen but I can feel it when I touch it. My right side of the neck is paining a lot. My head also pains sometimes I think it is all because of the wrong posture I was sitting in. So can you please tell me how can I get rid of this?
I can’t say is it a muscle knot or something other, for example, an enlarged lymph node, so you may want to go and check this with a doctor. You can also try to improve your sitting posture.
I’ve had pain which feels as though it’s right on the left shoulder blade for almost a year now. It’s felt more when there is pressure applied on it. I also get twinges of what feels like nerve pain in my upper left chest (above heart). I’ve had a chest x-ray, and cervical MRI which were both clear. I’m going to physio for 4 months now and it doesn’t seem to be helping nor does the naproxen or propranolol that my GP prescribed me for anxiety as I’m constantly worrying about this. I’ve seen two different ortho doctors and they both tell me to keep with the physio. I’m at my wits end as the pain is almost now constant (especially in left scapula). Could massage therapy, a chiropractor or acupuncture be of any use, help would be appreciated.
Muscle twinges often occur due to anxiety and so can scapular pain that feels like pressure. I personally do not recommend any therapy you’ve suggested. You can try to fully concentrate on your work and think if you can improve your posture, especially when sitting. Every worry has its origin. If you are under stress, you can think what you need to cope with and what you can discard as unnecessary.
Thanks for the reply, even before I suffered from anxiety last year the pain in the left scapula area was there. The pain in the chest area could definitely be related with anxiety though. When I’m relaxed on holiday for example the pain doesn’t subside.
If you think it’s not (only) anxiety-related, you can try to think of different possible causes and exclude the ones you are sure they are not the case.
For example:
1. How/when the pain started and was it related to an injury or excessive exercise?
2. Does the pain ever goes away for a period of time or at night?
3. Could it be bad posture and does the pain subsides if you try to improve posture? Does the pain increase/decrease when you move your arms or twist/bend the body?
4. Could it be gas pain?
5. Did you have any imaging investigation (ultrasound, MRI) of the scapula?
6. Where exactly is the pain and is the area tender to touch and is there any visible or palpable lump or deformity?
If the pain is organic, it could arise from the muscles, scapula, ribs or a bursa beneath scapula.
I would say that massage could help you. I find it invaluable for myself as any pain will help to stiffen up muscles making them more painful. I find such a lot of relief when I have a massage. I pay £30 for an hours session once a fortnight. This is for an upper body massage. It hasn’t cured me but can relive me of pain for some time. Hope this helps.
Hello again,
So, I am over 2 years on from the first onset of pain and still I’m getting no relief whatsoever from the pain in the upper back around the scapula area.
The pain I get is also like a numb feeling In my upper arm when pressure is applied on it, around my funny bone is really sensitive more than usual, in my chest and under my left armpit around the rib area.
There is small lump around my left side under my armpit that moves about. I cannot sleep on my left side as the numb feeling gets so much worse. I have always slept on my front with my neck twisted to the right and my left arm stretched above my head. I imagine this could be a serious factor but I’m unable to sleep on my back as I snore and it wakes my partner.
I have had 3 mri’s, one cervical and 2 x brachius plexus. (one with arms by my side and other with arms raised and a dye injected into my veins)
I have been to a chiropractor for a few sessions (Pointless as all he done was crack my back and neck) which offered no relief, so I then tried an osteopath who tried some acupuncture and massaging of the muscles and nerves around the places where it hurt. I gave up after about 5 sessions as it was costing too much with little relief.
I’ve tried to wear a back brace to help my posture as I’m quite hunched and sit at a computer most of the day.
Any advise would be welcome.
Kind Regards
William
I have recently developed dull aching pain in the rhomboid muscles that are debilitating and suck all energy away. This causes my mood to lower and a certain level of anxiety. Is there any medication that can be taken to assist with this pain?
You can try to improve your posture or avoid eventual repetitive or forced movements that cause this pain. Analgesics or muscle relaxants are usually not of much help.
I was at work … fuling for about 1 1/2 hrs…my chair too low for the table the file boxes were on…so think it was the reaching, stretching upward, motion (while filing) is 2hat caus3d my problem… 2 days later… my neck and shoulder was soooo sore when I awoke. The base of my skull… neck area has large swollen ridge … packed with sore, sore achy muscles…radiating pain to shoulder where there are nodules that are excrutiating to touch. Try massaging these “sore spots” (lumps) myself… have iced the areas… so far not much pain relief. Now will try heat. Any other suggestions?? I thought of getting muscle relaxant shots. But read here that will not work. At this point, I am just biting the bullet and putting up with the pain…hoping it will go away on its own in a few days!!!
I do have osteoarthritis… (degenerative joint disease)
Such symptoms can be due to:
– Wry neck or torticollis
– Delayed onset muscle soreness – a fancy term for muscle pain after excessive physical work (this should go away in few days)
– Stretched or even ruptured muscle (this may take more than a week to heal)
– A muscle cramp as a reaction to a painful condition in the neck (spine)
– Muscle knots as part of myofascial pain syndrome
Acute muscle pain is not relieved by heat but by cold (ice packs wrapped in a cloth and held at the painful site for ~15 minutes, few times a day). If the pain does not start to improve in a couple of days, visit a doctor.
I get tightness, tingling, numbness, weakness and a pinching feeling throughout the skin and when I touch muscles throughout my whole body. I have neck and should knots and tension that give me terrible head aches and tense my jaw all the time.
This sounds very similar to what I have been dealing with and I thought it was something very serious. I hope this is what it is so I can get help.
Is the diet for inflammation?
Thanks
I’m being tested for connective tissue disorders.
I don’t have any suggestions about the diet other than use your intuition about you think is good or bad for you.
Please help. 4 months now. I thought i slept wrong slight “kink” under my left shoulder blade. Weeks past and its painful to try to stretch arm and im now taking asprin. I can feel large tight knot form between shoulder blades. Had a friend rub my sore areas and she said she felt 3 small knots on both sides of my neck going down from my ears as well. Another knot and tightness at base of neck causing my neck limited side to side motion. A knot at base of skull which isnt as painful as everything else. Tightness to muscle above left collarbone. Pain at times shoots down left arm. When that happens it also feels like the knot under my shoulder blade is moving up towards neck. It causes pain like possibly pinching nerves? Can knots actually move? Hot pack helps. Hot goes away and i can feel it all tighten up again. Same with bengay. No accident. No heavy lifting. No stress. Just actually ended a week vacay filled with pain. I have an appointment for an hour message in 2 days. Any idea what im dealing with and what caused this for 4 months now?
Also the large knot at the base of my neck can be seen. I have a slight hump. No reddness or swelling. Painful. All feels bruises when rubbes.
A doctor will know better.
I shift my mower with my left leg. About an inch up from top of knee and on the inside. I’d take and lift leg and push that area to the right to shift mower. Spot was sore from doing and as I only mowed yards once a week I would do the same the following week even though was alittle sore. Now I have that pain there even though I stopped using that spot to shift mower. It hasn’t gone away on its own. It won’t hurt all the time. Sometimes when I get up quick it triggers it or the way a shift my weight while standing. It almost feels like nerve pain. The spot is real tender when it does start to hurt. Liquid Advil gels help and I have indocine I take for migraines which helps too but once the meds wear off the pain will come back. Any idea if something I can do to make it go away. 34 yr old male.
If it’s only a bruise or a stretched tendon it should go away on its own with time and relative rest of the leg. Ice packs help only in fresh injuries, probably within 48 hours. If the nerve is involved you would maybe feel some tingling or numbness down the leg, but again there’s not much to do to speed up recovery. If you think it’s something worse, you may want to visit an orthopedist.
Hi a continue of my last post with mower. It’s been a year and it hasn’t gone away. I don’t have medical insurance so I haven’t seen a doctor. I’m gonna try and see if I qualify to get on some kind of assisted medical because I can’t take it anymore. The lever to shift mower is kinda small but when I would shift once standing on mower the shifter would hit the same spot every time. I assumed it was just a bruise and would go away but it hasn’t. I started lifting leg and push lever with boot now. And it there has been a lot of down time since it first started hurting as we have winter season and don’t work. Thank you for responding to my post b4 and promptly. I appreciate it. My aunt mentioned to me that might need a small procedure where they would make a small incision and cut something. Maybe part of a tenden. Maybe it didn’t heal all the way and I kept shifting and the pressure on that spot b4 the bruise healed or whatever it is made it worse and turned it perminant. I have a commercial mower with a cart I stand on behind it. It has 5 gears. So once stand on it and hold brakes with both hands I kinda had to use my leg to shift and guy at mower shop recommended taking leg and pushing it. And it doesn’t push real easily but it’s not to hard to move it nether. Was enough to bruise me bad I guess. I should have stopped using that spot when first felt pain.
small tender knots in thighs (along IT bands on both sides and some in the front of thighs) and no where else. Dermatologist said not her area, orthopedic said look like lipomas and are not cancerous. Have multiple and not sure if these are trigger points or can they be relieved with ART and TP release?
If they are muscle knots, they can be probably relieved by some releasing technique.
So glad I finally found this I’ve been to my primary care doctor this weekend I went to the ER 2x’s they just look at me like I’m making something up they keep passing the buck no one wants to help me the ER physician wants my primary to send me to pain management without a diagnosis. I have painful knots on both sides of my stomach, thighs, outer sides of my arms, under my breasts, back, neck & back of my head not at the same time they happen at different times this weekend it was stomach, under my breasts, arms & it was very painful. What do I do now?
You can try to get an exact diagnosis by an orthopedist.
Help – I am a 50 yr old female, no prior injuries to the effected area’s. I have had upper back, rib area, right scapular now increasing arm pain for 5+ years with no diagnosis. Have had several MRI’s that do show mild deterioration of the cervical spine – consistent with age no trapped nerves. Neuro surgeon does not feel this is causing my issues. Nerve/Muscle conduction test DID show C5 nerve compromised causing muscle issues. Lot’s of conflicting reports and feeling very frustrated. As time has gone on feeling as if vision, balance and memory issues are arising. Constant muscle pain, inflammation (C-reactive tests ALWAYS Elevated) and knots, intermittent nerve sensations mostly in the rib, scapular, ribs and upper back area’s, feelings of itching or something crawling under my skin – also at times fells like it’s creeping around to the front bottom of my ribs in my belly area (doctor took gallbladder out in 2012 hoping that may have been the problem – Not the problem). I do see a massage therapist on a regular basis (at least weekly) however it seems that my pain is much worse between treatments. She recently discovered a lump next to my upper spine area in the region of the T4 – T5 that she does not feel is a muscle – said it feels more solid (however not bone). I am waiting to get in to the doctor to discuss further. I have NOT been able to wear a bra for several years as after having on on for just minutes my body starts aching and the pain is unbearable. It feels like the muscles on my bra line around my torso are going crazy. As soon as I take it off – it is INSTANT relief – however for day’s my body is super sensitive and wearing anything that may compress my muscles is unbearably uncomfortable. This is making life very difficult to manage – I lose strength in my right shoulder/arm within hours of EVERY day. Simple tasks like brushing my teeth, drying my hair are becoming quite difficult. I have battled this for so long now and feel very pushed off by doctors that I’m putting this out there for someone to PLEASE let me know if I’m missing something. Have been treated with the following: anti-depressants for pain management – no luck – Gabapentin for nerve issues – no luck – ice/heat therapy – physical & occupational therapy (they released me as it appeared to make my pain more constant and increased the severity). Orthapedic doc sent me to Neuro Surgeon as it was his belief that my cervical spine is the culprit – surgeon say’s no, pain management wanted to do cervical injections – I declined as family member is a medical chiropractor and reviewed MRI and Nerve Conduction reports and felt it was a reach.
I have a lot of popping and soft cracking sensations in my upper should area – constantly.
Health conditions: HBP – Raynauds – Barrets Esophagus
Any fresh input is appreciated and I am open to all suggestions!!
A bulging or herniated disc in the cervical spine that looks mild on MRI can cause significant pain. There are two simple tests that can tell if you have a herniated disc: 1. Put the hand of the affected side on top of the head. Pain relief speaks for a herniated disc. Arm pain aggravation may speak for thoracic outlet syndrome (briefly mentioned in the article about arm pain). Another test for herniated disc is Spurling test (your relative may help with this).
The report of the C5 conducting test maybe says at which point the nerve can be compressed – at the level of the spinal root or later in the course. Two common causes for C5 compression are a herniated disc or something other in the cervical spine and thoracic outlet syndrome.
I encourage you to get that newly discovered lump evaluated by an orthopedist or neurologist. Also describe the skin sensitivity to a neurologist. sensitivity
have you been evaluated for Ehlers Danlos hyper mobility syndrome
I am aware of trigger points. I have a few in neck & shoulders & lower back & have had them worked on for years. Did massage & acupressure every week for an entire year, still do acupressure a lot, got local anesthetic shots, dry needling g, acupuncture, meds, stretching, heat every day, you name it, I’ve tried everything I could think of & yet, the same ones are still there. I have herniations in my neck & low back, in addition to many other issues that showed up on MRI. I have Ehlers Danlos Syndrome also.
Anyway, at this point, when you have long, long term trigger points which haven’t responded to ANYTHING you’ve done, what are my final options? The one in my neck is literally the size of a ping pong ball & is so hard, it feels like an actual rock. Is there a surgical option when all else fails? I have to take strong pain meds just to live each day as a partial human being as it is, and I honestly suspect that my trigger points are actually more painful than the structural damage that showed up on MRI, bc of the location& feeling of the pain & it’s worsened state upon certain, or sometimes just about any, activity. Thank you
SuzyQ, I do not have a definite answer, but I have a strong feeling that in your case, the trigger points and muscle knots develop as a reaction to painful conditions, such as herniated disc. Even if the original pain is not that bad, you have probably adopted some forced upper body positions as an attempt to avoid the pain, and these positions are possibly contributing to muscle knots.
What you can do is to treat the pain from the original conditions as possible. Next, you can reconsider all the treating techniques (dry needling, acupressure…) because it is possible that all this constant attention you give to muscle knots is just aggravating the situation. It sounds like it has partly become a psychosomatic problem.
If you think about surgery – the surgery of the herniated disc (or other organic conditions) can help, but not likely the surgery of the muscle knots. Muscle knots are not a structural problem, but a sort of localized increased muscle tension.
You can ask an experienced orthopedist if the following can help:
1. Surgery of the herniated disc
2. A special type of massage called myofascial pain release
at age 14, after playing Viola for 6 years and during a period of long orchestra rehearsals, I woke up and took a shower. Washing my hair caused a sudden cramp so bad that my left shoulder and neck made me resemble someone with MS. The shoulder was drawn up and the neck down until they touched. The debilitating part ended in 3 days, but the cramp from the middle of the inside of my left shoulder blade, which extended to the neck lasts until this day, 50 years later. I eventually was diagnosed with fibromyalgia with trigger points evident in many places on my body.
I have tried through the years physical therapy and chiropractic manipulation which make the nerve more irritated, acupuncture which works on other problems except that area which is made worse by either it or electrical stimulation. If I get in an argument or severe stress the cramp is so bad it radiates up to the base of my skull. Yoga, etc. provides great temporary relief, but that muscle won’t relax at all and I am right back in the same boat within an hour. I finally relied on tramadol at max dose for 10 years which masked the pain a bit, but became less and less effective of course, and I asked my doctor for a plan to stop taking them completely. I have decreased my tramadol dose by one half already, and will be completely off it in a couple of months.
After a surgery I was given a morphine drip which made evrything numb except the cramped area. Muscle relaxants don’t work. In rhe past I have wondered if it is a variety of MS. It takes 5 minutes at bedtime to find a position for my neck which will allow me to sleep.
If anyone has any idea of what else to try, or can pseudo-diagnose what may be happening I would appreciate it, as I have gotten totally sick of just trying to ignore it.
The 2 things that provide the most relief are a combination of (1) Arnica-based gel or cream ( homeopathic, but in 64 years the best non-prescription muscle pain cream on the market, is odorless and takes about 20 minutes to work) and (2) Medical THC. I am currently trying CBG component but as of yet it hasn’t worked (started yesterday) but I hear it takes awhile before it starts working. I haven’t seen a Doctor yet who will admit to knowing about Arnica gel. I can buy it at any of the usual US drugstores, but never find it at Kaiser hospital or any other hospital’s non-prescrition shop. Arnica has been in use in Europe for centuries succesfully. I know of no side effects other than a few people develop a skin rash which dissappears with cessation. My 96 years old Mom tried it when she broke her hip and got pain relief. Every single person I have told about my experience with Arnica has tried and founnd some relief. It only works on me for a couple of hours, as does THC (well, 3 hrs sometimes) and I don’t know if it is more expensive than other common muscle pain rubs.
Since THC is the only drug in my personal history that quiets the nerve involved I find it a travesty that it is not available in every state. I don’t like feeling stoned or out of control, and smoke 1 toke each time which alleviates my pain completely without affecting my mental acuity except when I first try a new “brand”, or for the first 2 or 3 weeks after I started the therapy.
Everyone is an individual, and I would have never started this without first being honest with my Doctor and asking his opinion.
There is a great deal of evidence that THC is addictive both physically and psychologically. I take other meds every day which are “non-addictive” which bothered me more when I quit.
I just flew to a State where it is illegal for a week and couldn’t get THC. I think I went through either withdrawals or that the quick change in combination with my other meds did it, but I felt terrible. In spite of this, and whether it is addicting or not, to find something after 50 years which works has convinced me that the “trade-off” is worth it. Nobody else in my family does THC or has in the past that I know of. Their reaction has been mixed, some congratulating me, some still stuck on the past illegality of it. My wife is originally from S. Korea where THC possesion is a very serious crime, though for many drinking themselves silly every night is evidently socially acceptable. Because of this, she hates the fact that I use THC even though the only way she knows is by the smell. I love every member of my family beyond comprehension, especially my wife, but I will continue what works for me, and trust that their level of understanding will improve with time.
What I mean, is that if you decide to try it you can expect to have to deal with friction.
I must be clear that each of us is an individual with different needs and different solutions. I am NOT making a medical recommendation, just telling my personal story. I have no connection in any way, shape or form with either a THC producing company or Arnica gel maker.
It was difficult to write this, as I know it may cause me professional or personal troubles with others, but the benefits I have experienced from Arnica and THC make “coming out of the THC closet” imperative.
Any ideas from others would be greatly appreciated, and I am open to any other solution which works as well with as few side-effects.
Best of luck, and/or God Bless You depending on your preferences,
Frederick, my personal opinion is that such pain can be relieved by dealing with stress.
This is what happens when you get replies from a quack who thinks they know it all. Frederick, have you tried acupuncture and message therapy? I believe in doctors when I need them, but I have taking meds and side affects..Not that I don’t think they are needed, but if I can find something else, I will give it a try. I love my chiropractor, but I find that if I combine chiro with acupuncture and massage therapy, much more affective. I have never found physical therapy to be affective for myself.
I am 17 and have a very painful knot in my back on the left side towards the middle. I thought it could have been from the way I slept as I woke up with it. The next night I tried sleeping flat on my back to see of that would help. I have been applying a heating pad and stretching it for 2 days. Today is the third day I have had it and the pain is radiating up towards the back of my neck on the side of the pain. I also tried ibuprofen and massaging it but that has not helped either. I’m not sure what to do about it but it has affected my sleep and everyday chores.
Sienna, if it is a muscle knot it may be from some repeating exercise or the way you sit maybe? A knot may resolve with rest. If it does not go away soon, you may want to ask a doctor for diagnosis.
woke up with pain to left medial scapula, deep, throbbing, no relief with NSAIDS, when i press on the specific area it hurts but feels good at the same time; some associated shoulder pain down the arm with wrist pain and weakness. was on cumpture the day before for approx 6 hours straight….can this be this syndrome?
Michele, all I can say: both the scapular pain and the wrist pain can be from the computer. The increased sensitivity near the scapula is probably from the muscles/tendons around the scapula. The wrist pain can be a part of the carpal tunnel syndrome, so the two pains may not be directly related, but they both seem to be from computer work. I was a bit concerned about the “throbbing.” Unless the pain resolves quickly with some rest, please consider to go to the doctor.
What about LDN therapy for Mps?
Dawn, I personally would not focus on LDN.
This is the most comprehensive site that has provided information that describes my exact experiences on one side of my arm/shoulder/neck which has been building up over last 3 months. Bookmarking ehealthstar.com 🙂
So far I’ve had acupuncture and massage with had greatly reduced the discomfort but I did not go back for regular treatments so… it came back and worsened. I just started using the Rhino roller every night and that is also helpful but there are so many trigger points that I am hoping physical therapy will also be prescribed.
I am scheduled to see an Orthopedic Specialist for hands and shoulders but they told me he will refer me to another doctor if my neck is part of the issue which did not make logical sense since they clearly are aligned. This article helped me become so much more informed. THANKS!
Nik, by saying that the neck can be a possible issue, the doctor maybe meant a herniated disc in the neck spine, which typically causes pain in the shoulder and upper arm.
I have lots of pain in my neck and it radiates down my arm. I like how you mention so causes could be because of poor posture. I work at a computer all day and I wonder if this could be a cause of my neck pain. I wonder if trigger point injections will help ease my pain. Thanks for the information!
I hope this gets an answer… what of someone who has EVERYTHING you’ve listed at once, since being very young. I am now 33 and remember intermittent pains in all the areas that are now constantly pained. Pretty much every symptom you described. Also, I have many lympomas and cysts in all my limbs, hands, neck, thighs, soft tissue between my breasts and armpit… (whatever that.. joint or muscle is that connects there) I’m in so much pain my family is falling apart and everyone hates me because I don’t look sick, and they don’t believe my limitations… they think I am lazy, selfish, a bad mom, a bad partner, a bad housekeeper…. My daughter is 9. I haven’t been able to hold her since she was two and I can’t handle my 13 year old sons heavy hugs… Do they think I choose this for myself?! For them??? So many other problems… anemia, menorgia, blood clots, OA in my hips, cervical spine, scoliosis, labreal tares, rotatory tears… Why is my body destroying itself???!!! I want my life SO BAD. I am fighting so bad… but…. I don’t know how much longer I can live like this… no good to anyone, with to empathy or mercy in sight.
Sharese, some of the troubles you’ve mentioned can develop as a reaction to eventual wrong attitudes you may have to certain things.
How dare you say that to someone, Jan! Sharee have you seen a rheumatologist? For years I was misdiagnosed as I had no history of psoriasis until my first outbreak at 33, and it wasn’t until I did my own research after my joints became inflamed at 45 that I found out I had psoriatic arthritis, but I had suffered from SI joint dysfunction, plantar fasciitis for years..All related. There may be an underlying cause to all your symptoms, but like in my case, a regular MD never puts it all together. I have had the same doctor for years, but I only about specific problems, so he is treating immediate symptoms, and it wasn’t until I did research myself that the whole picture came together and I asked to be referred the rheumatologist who confirmed all related to my psoriatic arthritis and pointed out things I had no idea had any relation to disease. Sorry you are suffering. Attitude does have a bearing on your health, but when you are at a low point, know that there are support groups…You just need a proper diagnosis so you can get busy being proactive, and don’t ever allow someone to beat you down.
I am having the Serratus Anterior Muscle Pain….. So bad that I cannot eat, sleep, walk hold my head up, drive, wash my hair, pick out my clothes for the day, etc. I am in so much pain I would rather be paralyzed. PLEASE HELP ME. I DON’T KNOW WHAT ELSE TO DO! My Dr gave me lidocaine shots and they only made things worse. I am begging you for your help or suggestions!!
Tami, you can visit a doctor again and ask if you maybe have some additional injury, a damage of the nerve (for example, the thoracicus longus nerve) and if you can get some other pain relief. But even the muscle strain alone can be quite painful. I can’t say more than the rest helps and pain should improve in some days and probably disappear in few weeks.
I have severe pain in the left side above elbow , look like a muscle knot and i had trigger finger in the same hand, and any special stretching i can do to get ride of this pain? Any advise?
Elizabeth, I suggest you to get that knot checked by a doctor.
I have pain on the right side of my middle back in the dorsal region close to where the muscle joins the spinal cord but not on the spinal region.
I got CT scan, MRI, X Ray and Blood tests done but there was no finding.
Doctors say that it is a posture problem due to my sitting job. I have tried physiotherapy, muscle relaxants and exercises but the pain exists in the same point for the past 8 months. Also, there are several instances of exertion where the pain can be felt in my right hand(right leg sometimes) with numbness and fatigue.
Recently, another doctor has prescribed me antidepressants telling me it may be due to FMS sort of thing. But I am not having tender points like in FMS.
Some advise will be helpful here.
Shreya, diagnosis of fibromyalgia can be made only if you have tender points on specific locations, as you mentioned.
The muscle origin of pain is possible.
You did not mention which specific exercise triggers tingling in an arm or leg and where the tingling is (from shoulder down or only forearm, inner or outer side..)
I got huge massive knots from my traps down to the bottom of my shoulder blade on the outer side of my back and on my neck. The exact same knots are on the opposite side of my back kneck n side. I have lumps in my calls my butt my fee lock up like a Charlie horse in my foot. I m in non stop excruciating pain. . Everywhere I have gone says lymphoma .. But reading all this everything is exactly what im going threw..
Will, lymphoma can causes lumps (enlarged lymph nodes) in the front or side of the neck, in the armpits and in the groin. Enlarged lymph nodes do not appear in the shoulder blade area or anywhere in the back, buttocks or calves.
Muscle knots would be possible, but this is internet, I can’t make a diagnosis of any kind. Muscle knots can occur after repeating excessive exercise or as a response to some painful condition. Lumps can also occur from other causes: rheumatoid arthritis, underskin abscesses…
If in doubt, visit a doctor .. a quick physical examination can reveal a lot. A simple blood test can confirm or exclude the possibility of lymphoma.
After 20 years of suffering from this. With much trial and error. I know for sure that the cause of this is food allergies. For me it is msg which I believe is poisonous to the body they put it in almost everything we injest as food. Including spices. I believe without a doubt that it is the underlying cause of many diseases. Thanks for killing everybody so good and making everyone racked with pain on top of it -whomever is responsable
Sharp (R) shoulder/arm rotational pull injury at work. 4/14. Clinic then referral to orthopedic due to constant Pain in upper back of Shoulder near 1st rib. Neck pain, numbness in arm and last 2 fingers of (r) hand.
Several Therapy/massage/stretching sessions.
7 times Dry needling
Brachial branch to reduce Neck/head pain c3,c4,c5
Stretching exercises, Tens, Neck traction machine
Initially Trapezoid muscles (R) locked.Deep Tissue Therapy slowly released groups of muscles.
Pain levels and Numbness have not improved.
Avg days(non-working) 4-6 levels, high pain days(non-working) 6-10, often lasting 3-4 days at a time.
Orthopedic Physician diagnosis still unclear – 10/15
Unable to work or do any task at home.
Any advice? 62 and never before ill or hospitalized and concerned with future.
Dalmer, you need to get a diagnosis (by an orthopedist or neurologist): what causes your condition. Bulging/herniated discs in the neck spine or spinal arthritis, or thoracic outlet syndrome are few possible causes. The therapies you’ve mentioned are more for pain relief not to treat the cause.
My age is 18 years old and from last three days i feel pain in shoulder espacially in my scapula and then pain move towards my triceps and pintching pain in my elbow and then continue to pinky finger.Also in right chest and middle of chest.And i am feeling difficulty to find knots..
fatima,
there are several possible causes of your pain; one can be muscle uveruse resulting in myofascial pain but it could be also a pinched nerve in the spine or “thoracic outlet syndrome,” for example. An orthopedist can give you a diagnosis and suggest the appropriate treatment.
I have this same pain with occasional numbness in my pinky and ring finger, and was diagnosed with “thoracic outlet syndrome “. I have been suffering with this for nine years. I have tried meds for pain, depression and anxiety. Nothing has helped. I hope your not in the same situation.
my daughter (46) is suffering from Myofascial nodes and pains thetre from. She is officew going and compelled by heavy works both in Office and domestic fronts.pain She has been advised to take amitrypline 10 mg at evenings. But what could relieve her pains both permanently and temporarily and instantly?
Vittalanand,
antidepressants may not be a good long-term solution, since they may lead to dependency. An experienced orthopedist or physiotherapist can teach her specific exercises. If possible, she would also need to avoid the causes, such as eventual forced body posture at work, repetitive moves…