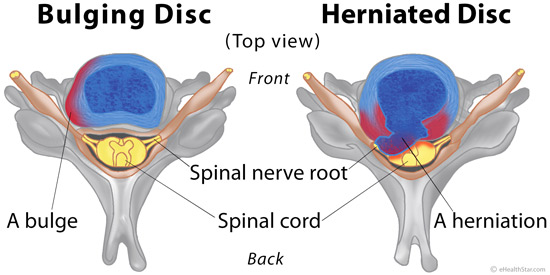
A bulging and herniated disc are two types of a damage of a spinal disc.
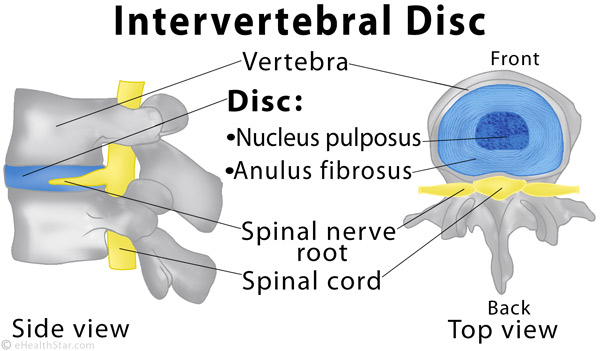
The spine is composed of the bones (vertebrae) and cartilages (discs) between them (Picture 1). An injury or wear and tear of the spine can result in a disc bulge or herniation, which can press on the roots of the spinal nerves and cause pain (Picture 2).
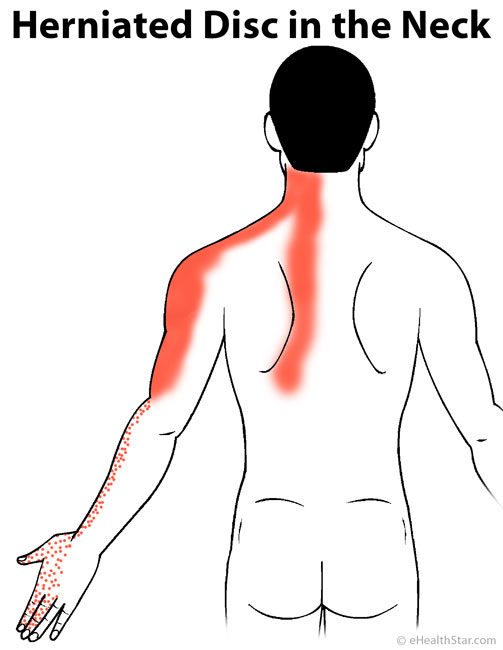
A compression of a spinal nerve root by a herniated disc is called a pinched nerve. A pinched nerve in the neck can cause pain in the neck and arm. A pinched nerve in the lower back can cause pain in the lower back and leg, known as sciatica.
Spinal Disc Anatomy and Function
Spinal or intervertebral discs are the cartilages between each vertebra in the spine, except between the 1st and 2nd vertebra in the neck and between the vertebra in the sacrum, which are fused together. The vertebra in the tailbone may or may not be separated by discs.
The discs are named by the two vertebrae they separate; for example, the disc between the 4th and 5th cervical vertebra is named C4-C5 and the disc between the 5th lumbar and 1st sacral vertebra L5-S1.
A disc has a firm outer fibrous ring (annulus fibrosus) and a soft, jelly-like center (nucleus pulposus) (Picture 1).
Picture 1. Spinal or intervertebral disc (blue)
The discs, which are relatively elastic, enable bending of the spine and act as shock absorbers.
Spinal Nerves
There are 31 pairs of the spinal nerves that emerge from the spinal cord [23]:
- 8 cervical nerves (C1-C8) in the neck
- 12 thoracic nerves (T1-T12) in the upper back
- 5 lumbar nerves (L1-L5) in the lower back
- 5 sacral nerves (S1-S5) in the pelvis
- 1 coccygeal nerve (Coc1) in the tailbone
The spinal nerves C1 to C7 emerge from the spinal cord above their respective vertebrae, for example, the nerve C1 emerges above the 1st cervical vertebra. The nerve C8 emerges between the vertebrae C7 and T1 and the remaining nerves (thoracic, lumbar, sacral and coccygeal) emerge below their respective vertebrae, for example, the nerve T1 emerges below the 1st thoracic vertebra (picture). The spaces between the vertebra through which the spinal nerves exit the spinal cord are called intervertebral or neural foramina.
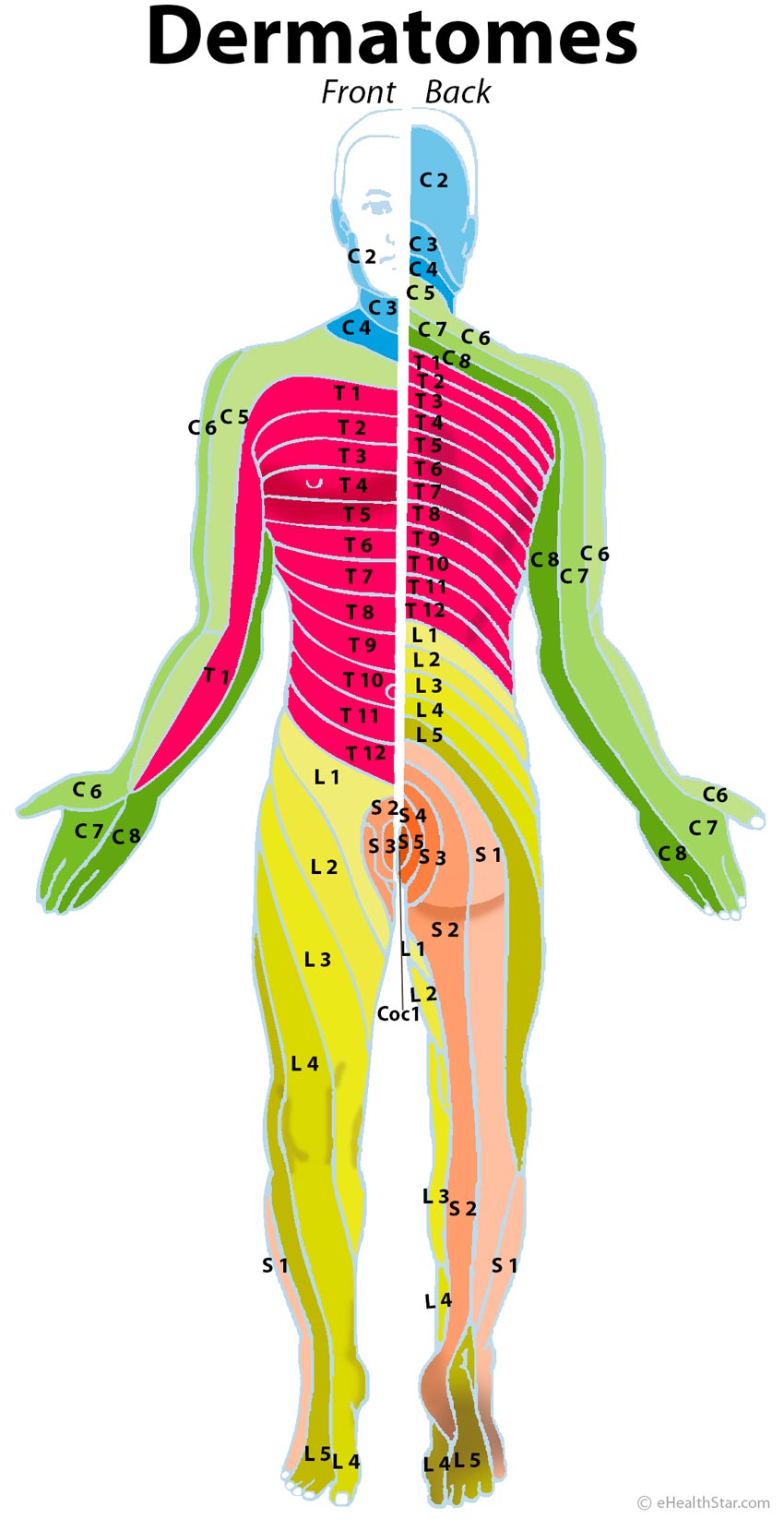
A herniated disc that presses on a particular spinal nerve root causes pain in the related skin area called dermatome. For example, a herniated disc between the cervical vertebra C5 and C6 that presses on the spinal nerve root C6 causes pain in the shoulder, the outer side of an arm and thumb (Chart 1 and Picture 4).
Bulging vs Herniated Disc
A bulging disc bulges out on one side but is not torn; it rarely presses on the spinal nerves or causes pain (Picture 2) [32].
A herniated disc has a torn outer ring through which the soft center squeezes out and can press on the spinal nerve root or spinal cord and cause pain (Picture 2) [32].
Picture 2. Bulging vs herniated disc
Causes and Risk Factors for a Bulging/Herniated Disc
The causes of a bulging or herniated disc include injuries of the spine and degenerative disc disease (DDD). Risk factors include a family history of disc disease, old age, excessive body weight, pregnancy, sedentary lifestyle, psychological stress and smoking [1,25,81].
Acute or Chronic Injury
Examples of causes of a bulging or herniated disc [4,31]:
- Acute injury during lifting a heavy object, fall from a height, car accident (whiplash injury)
- Strain of the spine due to repetitive prolonged sitting, driving, bending or heavy physical work
- Repetitive injuries in sports, such as weightlifting, football, rugby, skiing and diving
Degenerative Disc Disease (DDD) or Spondylosis
Degenerative disc disease (DDD) refers to wear and tear of the discs. With age, the discs lose some water and hence some shock absorbing capability, which makes them prone for herniation. However, DDD can occur in people as young as 20 years of age [4, anecdotal reports], which suggests that genetic and other factors also play a role in a disc damage [3,36].
Spondylosis refers to degeneration of the spine as a whole, which can include degeneration of the discs, vertebra and the joints between vertebra (spinal osteoarthritis) [35].
Symptoms
A bulging disc rarely causes pain or other symptoms.
Symptoms of a herniated disc:
- Discogenic pain arises from a torn or inflamed disc; it appears as deep, aching pain in the neck, upper or lower back on both sides of the spine, but not in the limbs [63].
- Radicular pain arises from a pinched or inflamed nerve root; it is burning, shooting, electric-like pain in the upper or lower limb on one or both sides, which can be associated with abnormal sensations (tingling and numbness) and muscle weakness [63,66].
- Painful muscle spasm in the neck or lower back lasting for several minutes appears as a reaction to a pinched nerve [2,67].
You may or may not feel a herniated disc. A small disc herniation may cause severe pain, and a large herniation may cause no pain [58]. The pain tends to be recurring and come in flares that can last from few days to few months [10].
Commonly associated symptoms are depression and weight loss due to loss of appetite caused by pain.
Diagnosis
A doctor can often make a diagnosis of a herniated disc from your medical history and physical examination [81].
X-Ray
An X-ray is a routine investigation in individuals with neck or back pain that does not improve after 6 weeks of physical therapy and when a surgical therapy is planned [54]. An X-ray cannot show a bulging or herniated disc but can show other spinal disorders, such as narrowing of the space between the vertebra due to disc collapse, spondylolisthesis, bone spurs (osteophytes), fractures, infection (osteomyelitis) and tumors [7,52].
MRI
A doctor usually orders magnetic resonance imaging (MRI) before surgery for a herniated disc in the neck [66] or lower back [7,52,53]. When surgery is not planned, an MRI may not be necessary. An MRI with contrast (gadolinium) can better show nerve root inflammation than a regular MRI [52].
Terms used in MRI reports to describe bulging and herniated discs and related disorders [52,59,99]:
- Disc desiccation means disc dehydration, which appears as “dark disc” on an MRI.
- An annular tear or fissure is a crack in the outer fibrous ring of the disc.
- A disc bulge is an extension of at least 25% of the disc’s circumference beyond its normal limits but the inner soft part of the disc is not squeezed out through the fibrous ring.
- Diffuse disc bulge is a general term for a disc bulge, which does not have more specific meaning that a disc bulge.
- A circumferential bulge means an extension of 50-100% of the disc’s circumference.
- A symmetrical bulge means an extension of 100% of disc’ circumference.
- An asymmetrical bulge means an extension of more than 25% but less than 100% of the disc’s circumference.
- A minimal disc bulge only slightly extends over its normal limits and does not put pressure on the nerve roots.
- A disc herniation (prolapsed, slipped, torn or ruptured disc) refers to the squeezing of a portion of the soft disc center through a crack in the fibrous ring.
- Focal herniation occupies less that 25% of the disc’s circumference.
- In a disc protrusion, the base of a herniation is wider than its top, and in disc extrusion, the base is narrower than the top.
- Broad based herniation occupies 25-50% of the disc’s circumference.
- Contained herniation is covered by the fibrous ring but uncontained herniation is not.
- Posterior or central herniation points backward to the spinal cord [59].
- Paracentral herniation points backward and slightly to the right or left but not toward the spinal nerve root.
- Posterolateral herniation points backward toward the right or left nerve root and can pinch it [59].
- Foraminal herniation points toward an intervertebral foramen – a space between the vertebra through which a spinal nerve exits the spine.
- Far lateral herniation extends beyond the intervertebral foramen; it can pinch a nerve on the same, upper or lower spinal level.
- Intravertebral herniation protrudes vertically into the upper or lower vertebra.
- Disc migration means the movement of a part of a disc to the higher or lower spinal level than the one of the original disc.
- In disc sequestration, a fragment of a disc loses the connection with the main disc body.
- Soft disc refers to a recent disc herniation without bone spurs, usually due to an injury.
- Hard disc refers to chronic disc herniation with bone spurs, usually due to long-term degenerative disc disease.
- Focal herniation occupies less that 25% of the disc’s circumference.
- A collapsed disc is a shallow disc that has shrunk vertically.
- Spinal stenosis is a narrowing of the spinal canal (the space with the spinal cord), for example, due to a herniated disc: 1/3 narrowed canal = mild; 1/3-2/3 narrowed = moderate; >2/3 narrowed = severe spinal stenosis.
Both false positive or false negative MRI results are possible: disc changes that seem to be severe on MRI may cause no symptoms and changes that seem to be mild may cause severe pain [7,10,54].
CT Scan With or Without Myelogram
Computed tomography (CT) can often show bulging and herniated discs equally well as MRI [81]. The advantage of a CT is a lower cost, and the main disadvantage is a high radiation exposure.
Herniated discs, especially those in the thoracic spine, often contain calcium deposits. A CT can show calcium deposits better than MRI, so it may be an appropriate investigation when a herniated disc in the thoracic spine is suspected [52,55]. Calcification of the discs can also occur in ankylosing spondylitis and some other spinal disorders [57].
A CT with myelography involves an injection of a contrast substance into the spinal canal following by a CT. A doctor can recommend this investigation before surgery, when spinal stenosis, spinal damage after trauma, multiple herniated discs, spondylolisthesis or a tumor is suspected, or when an MRI is not available, too expensive or contraindicated (in claustrophobia) [52,54,56,66]. The main side effect of myelography is a severe headache after the procedure [56].
Nerve Block
A nerve block involves an injection of a local anesthetic near the spinal nerve that is suspected to cause pain. Pain relief after an injection speaks for a pinched nerve as a cause of pain. A nerve block can be tried when an MRI or CT does not reliably confirm or exclude a pinched nerve [66].
Discography
Discography involves an injection of the saline solution into a disc that is suspected to cause pain. Pain after an injection that is similar to your existing pain speaks for a disc damage [52]. Discography can be done when other investigations do not reveal any damage to the nerve root that could cause pain [52]. The test is not considered very reliable and is now rarely performed [55].
Electromyography (EMG)
Electromyography (EMG) is a test of the muscle function; the function of a particular muscle is decreased when the nerve that supplies it is pinched by a herniated disc. EMG can be done when an MRI shows a herniated disc but it remains unclear if the disc is a cause of pain. When both an MRI and EMG are positive, the disc herniation is very likely the cause of pain [54,58]. There is insufficient evidence of the usefulness of an EMG in differentiating a herniated disc in the neck from other causes of neck pain [66].
Laboratory Tests
Herniated discs and pinched nerves by themselves do not cause any typical changes in the blood or urine tests [54]. A doctor can order certain blood tests, such as sedimentation rate (ESR), C-reactive protein (CRP), rheumatoid factor, immunoglobulins and white blood cells to check for eventual other causes of neck or lower back pain, such as rheumatoid arthritis, ankylosing spondylitis, cancer or kidney inflammation [55].
Treatment
1. Physiotherapy
There is insufficient evidence of the effectiveness of physiotherapy in reducing pain or long-term outcome of herniated discs [81,82].
2. Medications
Analgesics that may relieve pain in a herniated disc [9,35,63]:
- For acute mild or moderate pain:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): aspirin, celecoxib, diclofenac, diflunisal, etodolac, flurbiprofen, ibuprofen, ketoprofen, ketorolac (for max 5 days), mefenamic acid, meloxicam, naproxen, piroxicam or sulindac. Different individuals react differently to various NSAIDs.
- Oral glucocorticoids (steroids): prednisone for 1-2 weeks. Steroids can help in pain but they do not seem to improve the course of a disease.
- For severe acute pain lasting <2 months:
- Tramadol or narcotics (opioids), such as codeine, hydrocodone, oxycodone, propoxyphene for a short time
- For chronic pain:
- Acetaminophen
- Duloxetine
- Tricyclic antidepressants (amitriptyline, doxepin)
- For muscle spasms:
- Muscle relaxants cyclobenzaprine or orphenadrine
The anticonvulsants gabapentin may help in both radicular [88] and discogenic [89] pain but can have significant side effects, such as dizziness, dry mouth, nausea and headache.
According to one 2007 review of studies, there is insufficient evidence of the effectiveness of medications in reducing symptoms or long-term outcome of a herniated disc [81].
3. Surgery
Indications (reasons) for surgical treatment of herniated discs [1,58]:
- The presence of spinal stenosis
- Lack of effect of conservative treatment for 6-12 months or progressing worsening of symptoms
- Red flag (emergency) indications: bladder or bowel incontinence, progressive neurological problems, excruciating pain or sensory loss between the legs (in the perineum)
In general, surgery for a herniated disc is more effective in relieving arm or leg pain than neck or lower back pain [60].
Types of surgery:
Discectomy is a surgical removal of a herniated part of the disc [84]. According to one source, discectomy in the lower back has a high success rate when the herniation is more than 8 mm wide and a low success rate when it is less than 5 mm wide or when the pain in the leg is greater than the pain in the lower back [58].
- Open discectomy is a removal of a part of the disc through an incision in the front or back of the neck or in the lower back.
- Microdiscectomy is a discectomy with the help of an operating microscope inserted through a small incision.
Spinal fusion includes a total removal of one or more discs and their replacement with bone grafts from your pelvic bones (autograft), from another person (allograft) or with a synthetic disc [12,60,79]. Spinal fusion with instrumentation includes using metal screws, rods or cages, which may be later removed. The downsides of the spinal fusion are reduced mobility of the spine and increased risk of herniation in the adjacent discs.
Laminectomy or spinal cord decompression is a removal of the rear part of a vertebra called lamina to widen the spinal canal and reduce the pressure from a herniated disc or bone spurs on the spinal cord [79]. The surgical approach is from the back of the neck or lower back. Lumbar laminectomy is often effective in those with leg pain, but less likely in those who have only pain in the lower back [60]. Laminoplasty is a reconstruction rather than removal of the lamina [79].
Foraminotomy and foraminoplasty are two techniques used to widen one or more intervertebral foramina (openings between the vertebra through which spinal nerves exit the spine) in order to decompress a pinched nerve [86].
Corpectomy is the removal of all or a part of the vertebral body (corpus), usually along with two adjacent damaged discs [79,87].
Total disc arthroplasty or artificial disc replacement means the replacement of a damaged disc with a synthetic disc (prosthesis) [12,60].
Minimally invasive surgery includes different outpatient procedures that can be done under local anesthesia. NOTE: Some of these procedures are still in the experimental phases and may have a higher recurrence rate than classical surgical techniques.
- Laser discectomy involves a burning of a central portion of the disc by a laser conveyed through a needle inserted into the back of the neck or lower back [85].
- Percutaneous endoscopic lumbar discectomy (PELD) or nucleoplasty involves insertion of an endoscope through the skin in the lower back and cutting a damaged part of a disc [90,91].
- Chemonucleolysis involves an injection of a chemical that destroys the inner part of the disc [94].
- Intradiscal electrothermal therapy (IDET) [35] and disc biacuplasty [93] involve the destruction of a damaged part of the disc by heat introduced by a catheter inserted through the skin [35].
Surgery Complications
Complications of surgery for a herniated discs are rare but can include [60]:
- During surgery: an injury to a nerve root, spinal cord, neck or abdominal organs
- Days/weeks after surgery: infection of the operative wound, disc or vertebra, spinal stenosis, sacroiliac joint syndrome, myofascial syndrome, cauda equina syndrome, thrombophlebitis, pulmonary embolism or, rarely, paralysis, stroke or death
- Months/years after surgery: herniation recurrence in the same or adjacent disc
Herniated Disc In the Neck (Cervical Radiculopathy)
Cervical radiculopathy (Latin cervix = neck, radix = nerve root; pathy = disease) refers to pain due to a pressure of a herniated disc in the neck on the root of a spinal nerve in the neck.
The most commonly herniated discs in the neck are the one between the 5th and 6th cervical vertebra and the one between the 6th and 7th cervical vertebra [29,41].
Picture 3. Typical pain distribution in
a herniated disc in the neck spine
Symptoms of a Herniated Disc In the Neck
- Pain at the back of the neck or head (occipital neuralgia) or between the shoulder blades, and neck stiffness [27,29,42].
- Pain, tingling, numbness or weakness in the shoulder, arm, hand or fingers on one or both sides [26,27,29,33].
- The pain may be aggravated by bending the head backward or tilting it sideways [26,27,68].
- The pain may be relieved by lying on the back [33] but may be worse in the morning [68].
Chart 1. Symptoms of Pinched Nerves In the Neck and Upper Back |
|||
Spinal Nerve |
Segment (Disc) |
Pain and Paresthesia Distribution (Dermatome) |
Affected Muscle Functions |
| C2 | C1-C2 | Back of the head, ear, the angle and bottom of the jaw | Bending the neck forward and backward |
| C3 | C2-C3 | Back or front of the neck; pain behind the eyes | Tilting the head toward the shoulders |
| C4 | C3-C4 | Base of the neck, upper part of trapezius muscle | Elevation of the shoulders (shrugging) |
| C5 | C4-C5 | Collar bones, front of the shoulder, base of the neck, the outer side of the upper arm | Raising an arm forward or sideways |
| C6 | C5-C6 | The back and outer (lateral) side of the shoulder, upper part of the shoulder blade, outer side of the upper arm and forearm, the thumb | Raising an arm forward, backward or sideways |
| C7 | C6-C7 | Shoulder blade or between the shoulder blades, back of the upper arm and forearm, 2nd and 3rd finger and the related part of the hand | Wrist flexion and extension |
| C8 | C7-T1 | Shoulder blade or between the shoulder blades, inner side of the upper arm and forearm, 4th and 5th finger and the related part of the hand | Bending the fingers |
| T1 | T1-T2 | Upper part of the shoulder blades, upper chest, inner side of the upper arm and forearm | Spreading the fingers |
| T2, T3 | T2-T3, T3-T4 | Lower part of the shoulder blades, upper chest, armpit (axilla) | |
| T4 | T4-T5 | Back and chest at the breast nipples level | |
| T5-T9 | T5-T6 to T9-T10 | Below the shoulder blades, flanks, between the nipples and the belly button | |
| T10 | T10-T11 | Lower back and abdomen at the belly button level | |
| T11, T12 | T11-T12, T12-L1 | Lower back, above the hips, abdomen bellow the belly button | |
Chart 1 sources: [18,19,20,22,24,29]. NOTE: There may be a considerable overlapping between dermatomes or an absence of any specific pattern; nerves on multiple levels can be pinched [66].
Physical Examination: Provocative Tests and Signs
- Shoulder abduction. While sitting, place the hand on the affected side on the top of the head; pain relief in the arm speaks for cervical radiculopathy [26,28].
- Valsalva maneuver. Take a deep breath, pinch your nose and forcefully exhale through it for 2-3 seconds; pain radiating down the arm suggests a herniated disc [28]. The test is often false negative (no pain despite the presence of a herniated disc) but is highly specific (the pain speaks for a herniated disc and not some other disease with a great certainty) [98].
- Spurling’s test. You sit with the neck slightly extended backward and rotated to the painful side. A doctor applies a downward pressure on your head: if you feel pain radiating down your arm, it is very likely you have a pinched nerve in the neck [27,44,69].
- Palpation. Tender points along the neck spine and the medial shoulder blade border or in the upper arm can result from a herniated disc [27]. Trigger points in the neck and upper back that elicit pain in distant body areas upon pressing were found in 51% of individuals with cervical radiculopathy in one study [78].
Complications of Herniated Discs In the Neck
A large disc herniation in the neck can cause damage to the spinal cord (cervical myelopathy) possibly resulting in weakness of both legs (paraplegia), both legs and arms (tetraplegia), bladder incontinence or recurrent urinary tract infections [61].
Differential Diagnosis for Cervical Radiculopathy
Conditions that can mimic cervical radiculopathy [34,36,43]:
- Muscle conditions:
- Wry neck or torticollis
- Cervical sprain and strain or whiplash injury
- Cervical myofascial pain
- Rotator cuff injury or adhesive capsulitis (frozen shoulder)
- Fibromyalgia (tender points, fatigue)
- Polymyalgia rheumatica
- Polymyositis and dermatomyositis (muscle weakness, skin rash)
- Neurological conditions:
- Carpal tunnel syndrome
- Thoracic outlet syndrome and other disorders of the brachial plexus
- Neuropathy due to diabetes, alcoholism or vitamin B12 deficiency
- Shingles (itchy rash)
- Transverse myelitis–an inflammation of the spinal cord due to autoimmune disorders, such as multiple sclerosis, rheumatoid arthritis or SLE
- Complex regional pain syndrome (CRPS) [63]
- Syringomyelia – a cyst in the spinal canal
- T4 or upper thoracic syndrome
- Bone conditions:
- Rheumatoid arthritis or systemic lupus erythematosus (SLE) [28]
- Spinal osteoarthritis or cervical facet syndrome
- Discitis (an infection of a disc), usually associated with osteomyelitis (an infection of a vertebra)
- Paget’s disease of the bone
- Other:
- Coronary heart disease with angina pectoris
- Tumors [63,68]: a tumor in a nerve root (schwannoma), Pancoast tumor (cancer at the top of the lung), thyroid or esophageal cancer, lymphoma
Treatment Options for Herniated Discs In the Neck
Conservative, natural treatment (partial rest, immobilization, physical therapy) alone without any medications or surgery is very often successful in the treatment of cervical radicular pain [62,63,64]. Symptoms may improve spontaneously within few months without any specific treatment at all [66,74,76].
1. Partial Rest
Individuals with a recent cervical radiculopathy should avoid excessive neck movements [74]. Bed rest is usually not needed.
2. Immobilization: Cervical Collar
A cervical collar is intended to limit neck movements and thus speed up recovery in individuals with acute cervical radiculopathy. A soft or semi-hard cervical collar during the day for 1-3 weeks and partial rest is often associated with faster pain relief than rest alone [74,75]. NOTE: A long-term collar use (>1 month) can weaken the neck muscles and postpone the recovery [63].
3. Home Remedies
- Moist heat pads or ice packs can help relieve acute pain [61,63].
- Molded cervical pillow at night can help prevent excessive neck movements.
- Adjusting a desktop or using an ergonomic chair can help improve body posture [8].
4. Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin or ibuprofen, and opioids, such as morphine (in severe pain lasting <8 weeks) may help relieve the pain [63].
5. Physiotherapy and Exercise Programs
Physical therapy and relative rest for 6 weeks can reduce acute neck and arm pain more efficiently than rest alone [74,75] but does not necessary affect the long-term course of a disease [68].
Therapy in the first 6 weeks (3-5 times a week) after the onset of pain can include [63,68]:
- Neck-school: a small group education and stretching exercises within the painless range of motion of the neck [63]
- Neck massage
- When the pain improves: graded strengthening exercises, such as chin-to-chest, side-to-side swivel, eyes-to-the-sky and ear-to-shoulder [11]
A good sign of the effectiveness of exercise is a gradual movement of symptoms from the arms toward the spine (centralization); the movement of symptoms from the spine toward the arms (peripheralization) speaks for wrong exercising regime or poor body posture [62].
6. Surgery
Surgery can be considered when severe pain, muscle weakness or neurological signs persist after 6 weeks of conservative therapy [63]. Surgery can provide quick pain relief, but long-term results may not be better than with conservative treatment alone [80].
Surgical techniques with an approach from the front of the neck include anterior cervical foraminotomy (ACF), anterior cervical discectomy (ACD), or corpectomy, anterior cervical discectomy with vertebral fusion (ACDF) and cervical total disc arthroplasty (TDA). Techniques with an approach from the back of the neck include laminoplasty, laminectomy and posterior foraminotomy and/or discectomy [62,65,66].
Recovery time after surgery [95]:
The recovery time depends on the extent of damage to your spine and the type of surgery, but in general, you can expect:
- 1-2 days stay in the hospital
- Return to work within a week
- Wearing a cervical collar for a week or longer
- Difficulty swallowing or hoarseness for few weeks
- 4-6 weeks of restriction of activity and, sometimes up to 16-12 months of restriction of your neck movements
- Physical therapy with strengthening exercises from the week 4-6
7. Treatments With Insufficient Evidence of Effectiveness
Manual or mechanical traction provides only temporary relief and is not likely effective in relieving chronic pain lasting for more than 3 months [61,63].
Manual or mechanic spinal manipulation is either not recommended, or there is insufficient evidence of its long-term effectiveness [63,64,66,77]. Complications, while rare, may include further nerve root damage, myelopathy (spinal cord damage) and worsening of pain [63,64].
Epidural steroid injections may provide a short-term pain relief in individuals with an MRI-confirmed cervical radiculopathy [61,62] but may not improve the long-term outcome of the disease [44]. A rare, but serious complication is damage to the spinal cord or brainstem [63].
A selective nerve root block with a local anesthetic may relieve a headache in some individuals with cervical radiculopathy [67].
A cervical epidural nerve block may reduce pain due to inflammation of the discs or nerve roots [61,62].
Prolotherapy, which involves injections of a local anesthetic or steroid into the muscle knots, may relieve myofascial pain in the neck muscles [61].
Other treatments with insufficient evidence of effectiveness include acupuncture [66,71,73], yoga [71,72] and Pilates [72].
Dermatomes
A dermatome is a skin area from which the sensations travel to a particular spinal nerve root. Pain, tingling or numbness in a certain dermatome suggest which spinal nerve may be affected. For example, pain in the thumb and the outer side of an arm suggest that the spinal nerve C6 is pinched (Picture 4).
Picture 4. Dermatome map
C = cervical (blue and green); T = thoracic (red)
L = lumbar (yellow); S = sacral (brown); Coc = Coccygeal
Herniated Disc In the Lower Back (Lumbar Radiculopathy)
The most commonly affected discs in the lumbar spine are the disc L4-L5 and the disc L5-S1 [41].
Symptoms of a Herniated Disc In the Lower Back
- The first symptom is usually a deep aching pain in the middle of the lower back that often becomes better in few days.
- Later, a superficial burning or shooting pain and tingling (pins and needless) can appear in a buttock, back of the thigh and calf, and occasionally in the calf, foot or toes, usually only on one side [5,19,40,41,43]. The leg pain, known as sciatica, can be mild or severe and can occur with or without lower back pain; usually, the leg pain is more severe than back pain [43,81]. The pain location depends on which disc is affected (see Chart 2 below).
- In advanced cases, numbness and leg weakness can develop [19].
- Pain can be triggered by coughing, sneezing, bending, lifting heavy loads, sitting, vibration (driving), prolonged standing, lifting a leg forward and intense running [5,10].
- Pain can be relieved by lying on a side with bent hips and knees (fetal position) or with a pillow under the knees, by frequently changing position, walking or slow running [10,43].
- You may experience “cold foot symptoms” with a cold, pale and numb foot [97].
Chart 2. Symptoms of Pinched Nerves In the Lower Back |
|||
Spinal nerve |
Segment (Disc) |
Pain or Tingling Location (Dermatome) |
Affected Muscle Functions |
| L1 | L1-L2 | Lower back, hip, groin (inguinal region) | |
| L2 | L2-L3 | Lower back, hip, upper front and inner mid-thigh | Raising the leg forward |
| L3 | L3-L4 | Lower back, hip, a part of the front and inner thigh, medial part of the knee and calf | Raising the leg forward |
| L4 | L4-L5 | Lower back, outer thigh, front of the knee, inner lower leg, inner ankle, medial part of the foot, big toe | Raising the leg forward or backward |
| L5 | L5-S1 | Lower back, upper buttocks, outer thigh, knee, lower leg and heel, upper part of the foot, 2nd to 4th toe and the related part of the sole | Raising the leg backward and knee flexion |
| S1 | S1-S2 | Buttocks, back of the thigh, outer lower leg, outer ankle, outer part of the foot, 5th toe | Raising the leg backward and knee flexion |
| S2 | S2-S3 | Buttocks, genitalia (penis, scrotum), back of the thigh and calf, the inner bottom part of the heel | Spreading the toes and flexion the foot downward |
| S3, S4, S5 | from S3-S4 to S5-Coc1 | Around the anus, genitalia (penis and scrotum, vulva) and the area between the anus and genitalia (perineum) | (S3) Spreading the toes |
| Coc 1 | Coc1-Coc2 | Coccyx (tailbone) | |
Chart 2 sources: [18, 19,20,22,23,24]. NOTE: there may be some overlapping between dermatomes. Sometimes, radicular pain may not follow dermatomes at all [30,33].
Physical Examination: Provocative Tests and Signs
Palpation may reveal tenderness or trigger points near the lumbar spine.
Straight leg raise (Lazarevic test). You lie on the back and a doctor starts to raise your extended leg. The pain that occurs at the leg elevation between 30 ° and 70 ° and radiates from your lower back to at least below your knee speaks for lumbar radiculopathy [5,38,59]. The positive test (pain) does not confirm radiculopathy, but negative test (no pain) pretty much excludes it [39].
Lasègue test is similar to the straight-leg test and includes forced flexion of the foot during the leg raise [59].
In a crossed straight leg raise test, a doctor raises your unaffected leg; the pain that appears in your affected leg further speaks for lumbar radiculopathy [39].
Pelvic rocking. A doctor flexes your leg in the hip and moves it in various directions; the pain in your lower back or buttock speaks for lumbar radiculopathy [5].
A neurological examination may, rarely, reveal numbness, decreased muscle strength and impaired reflexes in the leg [5].
Valsalva maneuver, which involves exhaling against closed mouth and nose, may trigger pain in the lower back [92].
Complications of a Herniated Disc In the Lower Back
Spondylolisthesis refers to a forward displacement of a vertebra, usually by an injury or severe disc degeneration.
A large disc herniation can result in stenosis of the spinal canal with a compression of the spinal cord–myelopathy–with pain, tingling, numbness and heaviness in the hands and feet and, rarely, bladder and bowel incontinence and erectile dysfunction [45,63].
A large disc herniation in the lumbar spine can press on several lumbar nerve roots and cause the cauda equina syndrome – a medical urgency with bladder and bowel incontinence, bilateral numbness in the buttocks and inner thighs area (saddle pattern) and pain in the back of one or both legs [19].
Differential Diagnosis for Lumbar Radiculopathy
Conditions that can mimic lumbar radiculopathy [2,6]:
- Psychological stress (pain in the lower back, but not in a leg)
- Muscle strain or tendon/ligament injury [19]
- Shin splints (pain on the medial side of the lower leg triggered by running)
- Ankylosing spondylitis (stiffness and pain in the lower back and buttocks, worse in the morning, in young men) [48]
- Psoriatic spondylitis (inflammation of the joints in fingers and toes, low back pain, with/out skin psoriasis)
- Sacroiliac joint dysfunction (pelvic pain) [47]
- Hip disorders (pain in the hip, groin and front of the thigh)
- Piriformis syndrome [49]
- Reactive arthritis in males after urinary tract infection or sexually transmitted disease (pain in the lower back, knee, ankle and foot, inflammation of the eyes)
- Stress fracture of the 5th or 4th lumbar vertebra (spondylolysis) common in young athletes (sharp pain in the lower back at the waistline) [50]
- Compression fracture of the vertebra due to osteoporosis or bone cancer (sudden, disabling, knife-like pain in the middle or lower back) [51]
- Kidney disorders: kidney stones (sudden, extreme pain), infection or pyelonephritis (tenderness in one or both flanks, fever, cloudy urine)
Treatment Options for Lumbar Radiculopathy
There seems to be insufficient evidence of any treatment, including analgesics, physical therapy, spinal manipulation, steroid injections and surgery, that would result in better symptom relief 1-2 years after the onset of symptoms than no specific treatment at all [81,82].
1. Partial Rest and Home Remedies
After acute disc herniation with severe pain, bed rest from few hours to 7 days may provide some pain relief but does not result in faster recovery, so continuing with mild physical activity, like household work and walking, as soon as possible is recommended [2,81].
Moist heat pads and ice packs for 20 minutes several times a day can help relieve acute pain.
Back school — a small group education about spinal anatomy, herniated discs, proper lifting, improving sitting or sleeping position, etc. is recommended [35,81].
Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen, or stronger analgesics can help relieve pain.
Insufficient Evidence
There is insufficient evidence of the effectiveness of the following therapies in relieving pain from a herniated disc in the lower back:
- Intradiscal Electrothermal Therapy (IDET) and Radiofrequency Posterior Annuloplasty (RPA) are the treatment methods that involve a placement of an electrode into the disc [35].
- Inversion tables are popular, but there seems to be a lack of studies of their effectiveness. In one small 2012 study, fewer participants who were using inversion table needed surgery afterward than those who were not [70].
- Physical therapy
- Stretching exercises (walking over flat ground, pool therapy, swimming, hamstring stretching routine, psoas major stretch and abdominal bracing) may not be more effective than rest and ice packs [14,19,81,82].
- Massage may help relax tight spinal muscles [8,35].
- Lumbar traction may temporarily relieve pain in some individuals [35,81,82].
- Wearing back braces may weaken back muscles and make the problem worse [35,83].
- Spinal manipulation by a chiropractor may worsen symptoms [58,81].
- Ultrasound
- Transcutaneous electrical nerve stimulation (TENS) can provide some immediate, bur less likely long-term pain relief [35].
- There seems to be no evidence of the effectiveness of acupuncture [81,82].
- Injections of steroids and local anesthetics into the muscle knots may help relieve pain due to muscle spasms [19,81].
- Epidural steroid injections may provide pain relief lasting for few days or up to several months according to some [7,15,35,60] but not other sources [81,82].
Surgery
Surgical treatment of lumbar radiculopathy can provide fast pain relief but 1-2 years after the onset of pain there seems to be no significant difference between surgery and conservative treatment [81]. In about 20% of individuals, surgery does not relieve pain [94].
Recovery time. You can expect to get out of the hospital in about 2 days and get back to work in about a week after a low back surgery. Often, you can expect to be pain-free in about 6 weeks after surgery; you may still feel some tingling at 3 months and some numbness for up to about a year [96].
Living with a Herniated Disc
The following can help you avoid the recurrence of a herniated disc or its faster healing [8,11,60]:
- Avoid smoking and excessive alcohol drinking.
- If overweight, lose weight.
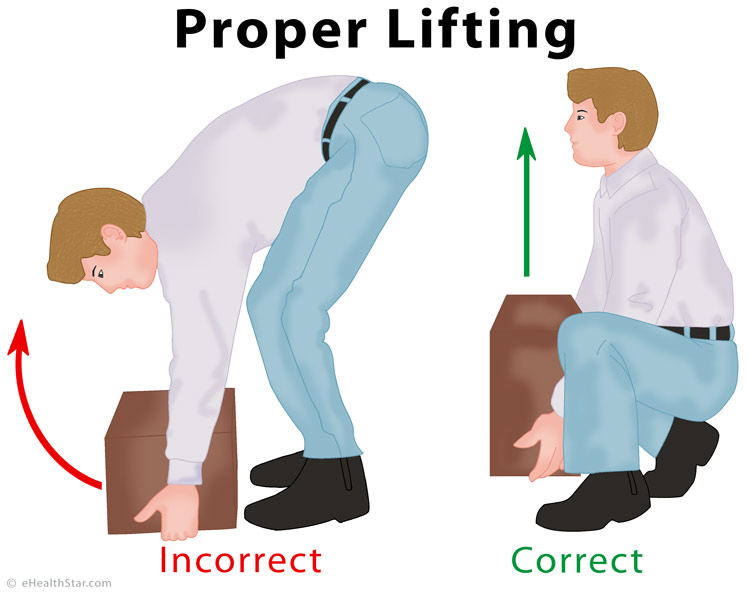
- Learn to lift objects properly.
- Improve bad posture.
Prognosis and Recovery Time
Often, the pain from a herniated disc goes away completely or becomes less severe in few weeks or several months just with conservative treatment (medications, physiotherapy) or without any specific treatment at all [25,26,81]. The herniated part of the disc can reabsorb (disappears) in 1-2 years on its own [31,44,59]. A disc that was once herniated and then healed is more vulnerable for subsequent herniations.
Prevention – Proper Lifting
The proper lifting of heavy objects can help prevent low back injuries including herniated discs. Keep your feet apart, with one foot behind the load and the other in front of it.
Picture 5. Proper lifting technique:
feet apart, straight back, lifting vertically
- References
- Kishner S, Degenerative disk disease Emedicine
- Pain from degenerative disc disease Spine-health
- Battié MC et al, 2004, Lumbar disc degeneration: epidemiology and genetic influences PubMed
- Patel RK, Lumbar degenerative disk disease Emedicine
- Patel RK, Lumbar degenerative disk disease, clinical presentation Emedicine
- Patel RK, Lumbar degenerative disk disease, differential diagnosis Emedicine
- Patel RK, Lumbar degenerative disk disease, workup Emedicine
- Patel RK, Lumbar degenerative disk disease, treatment Emedicine
- Patel RK, Lumbar degenerative disk disease, medication Emedicine
- Common symptoms of degenerative disc disease Spine-health
- Cervical degenerative disc disease treatment options Spine-health
- Surgery for a degenerated disc Spine-health
- Potential risks of surgery for a degenerative disc Spine-health
- Hamstring stretching exercises for sciatica pain relief Spine-health
- How epidural steroid injections work Spine-health
- Epidural injection procedure Spine-health
- Epidural injection pain relief success rates Spine-health
- Radiculopathies University of Wisconsin-Madison
- Humphreys SC et al, 1999, Clinical Evaluation and Treatment Options for Herniated Lumbar Disc American Family Physician
- Dermatome map of the body Backpain-guide.com
- Spinal cord and spinal nerve roots Spine-health
- Kishner S, Dermatomes anatomy Emedicine
- Overview of spinal cord disorders Merck Manual, Consumer Version
- Myotomes West Virginia University
- Herniated disk in the lower back OrthoInfo
- Cervical radiculopathy OrthoInfo
- Malanga GA, Cervical radiculopathy, clinical presentation Emedicine
- Provocative tests for cervical radiculopathy Air Neck Traction
- Cervical radiculopathy Air Neck Traction
- Murphy DR et al, 2009, Pain patterns and descriptions in patients with radicular pain: Does the pain necessarily follow a specific dermatome? PubMed Central
- Windsor RE, Cervical disc injuries Emedicine
- Furman MB, Cervical disc disease Emedicine
- Furman MB, Cervical disc disease, clinical presentation Emedicine
- Furman MB, Cervical disc disease, differential diagnosis Emedicine
- Middleton K et al, 209, Lumbar spondylosis: clinical presentation and treatment approaches PubMed Central
- Al-Shatoury HAH, Cervical spondylosis, differential diagnosis Emedicine
- Bulging disc American Spinal Decompression Association
- Liferidge A, 2011, Performing straight leg raise test for sciatica University of Maryland, School of Medicine
- Gregory DS et al, 2008, Acute Lumbar Disk Pain: Navigating Evaluation and Treatment Choices American Family Physician
- Lee-Robinson A et al, 2010, Clinical and Diagnostic Findings in Patients with Lumbar Radiculopathy and Polyneuropathy American Journal of Clinical Medicine
- Taylor LP et al, Neck and back pain American Academy of Neurology
- Mizutamari M et al, 2010, Corresponding scapular pain with the nerve root involved in cervical radiculopathy PubMed
- Hochschuler S, Sciatica symptoms Spine-health
- Voorhies RM, 2001, Cervical Spondylosis: Recognition, Differential Diagnosis, and Management PubMed Central
- 2013, Spinal stenosis National Institute of Musculoskeletal and Skin Diseases
- What is transverse myelitis Johns Hopkins Medicine
- Sherman AL, Sacroiliac joint injury, clinical presentation Emedicine
- Brent LH, Ankylosing spondylitis and undifferentiated spondyloarthropathy, clinical presentation Emedicine
- Shah S, Piriformis syndrome, clinical presentation Emedicine
- Spondylolysis and spondylolisthesis OrthoInfo
- Compression fractures of the back MedlinePlus
- Ramachandran TS, Disc herniation imaging Emedicine
- Windsor RE, Cervical discogenic pain syndrome, workup Emedicine
- Al-Shatoury HAH, Cervical spondylosis, workup Emedicine
- Kishner S, Degenerative disc disease, workup Emedicine
- Myelography Radiologyinfo.org
- Knipe H et al, Intervertebral disc calcification Radiopedia.org
- Lumbar disc herniation Chirogeek.com
- Lumbar disc herniation Orthobullets
- Kishner S, Degenerative disc disease treatment & management Emedicine
- Al-Shatoury HAH, Cervical spondylosis treatment & management Emedicine
- Albert HB et al, 2012, Centralization in patients with sciatica: are pain responses to repeated movement and positioning associated with outcome or types of disc lesions? PubMed Central
- Eubanks JD, 2010, Cervical Radiculopathy: Nonoperative Management of Neck Pain and Radicular Symptoms American Family Physician
- Boyles R et al, 2011, Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review PubMed Central
- Kyoung-Tae K et al, 2010, Cervical Radiculopathy due to Cervical Degenerative Diseases : Anatomy, Diagnosis and Treatment PubMed Central
- Bono CM et al, 2010, Diagnosis and treatment of cervical radiculopathy from degenerative disorders North American Spine Society
- Persson LCG et al, Headache in patients with cervical radiculopathy: a prospective study with selective nerve root blocks in 275 patients PubMed Central
- Cervical disc disease Family Practice Notebook
- Cervical disc herniation Wheelessonline.com
- Prasad KS et al, 2012, Inversion therapy in patients with pure single level lumbar discogenic disease: a pilot randomized trial PubMed
- Xu W et al, 2015, PubMed Central, Complementary and Alternative Medicine for the Management of Cervical Radiculopathy: An Overview of Systematic Reviews PubMed Central
- Sorosky S et al, 2008, Yoga and pilates in the management of low back pain PubMed Central
- Fu LM et al, 2009, Randomized controlled trials of acupuncture for neck pain: systematic review and meta-analysis PubMed
- Dmytriv M et al, 2010, PT or cervical collar for cervical radiculopathy? PubMed Central
- Kuijper B et al, 2009, Cervical collar or physiotherapy versus wait and see policy for recent onset cervical radiculopathy: randomised trial The BMJ
- Thoomes EJ et al, 2013, The effectiveness of conservative treatment for patients with cervical radiculopathy: a systematic review PubMed
- Rodine RJ et al, 2012, Cervical radiculopathy: a systematic review on treatment by spinal manipulation and measurement with the Neck Disability Index PubMed
- Sari H et al, 2012, Active myofascial trigger points might be more frequent in patients with cervical radiculopathy PubMed
- Kavanagh RG et al, 2012, Operative Techniques for Cervical Radiculopathy and Myelopathy Hindawi
- van Middelkoop M et al, 2013, Surgery versus conservative care for neck pain: a systematic review PubMed Central
- Koes BW et al, 2007, Diagnosis and treatment of sciatica PubMed Central
- Luijsterburg PAJ et al, 2007, Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review PubMed Central
- Herniated disc MedlinePlus
- Chin LS, Lumbar discectomy technique Emedicine
- Chawla J, Laser discectomy Emedicine
- Foraminotomy MedlinePlus
- Spoonamore MJ, Anterior cervical corpectomy and fusion University of Southern California
- Kasimcan O et al, 2010, Efficacy of gabapentin for radiculopathy caused by lumbar spinal stenosis and lumbar disk hernia PubMed
- Levis OS et al, 2009, Efficacy of gabapentin in patients with discogenic lumbosacral radiculopathy PubMed
- Zeng J et al, 2013, Complications of Percutaneous Endoscopic Lumbar Discectomy via Interlaminar Approach Society for Minimally Invasive Spine Surgery
- Mirzai H et al, 2007, The results of nucleoplasty in patients with lumbar herniated disc: a prospective clinical study of 52 consecutive patients PubMed
- Lewin KH, 2010, Low back pain Cleveland Clinic
- Kapura L et al, 2008, Intervertebral disc biacuplasty for the treatment of lumbar discogenic pain: results of a six-month follow-up PubMed
- Couto JMC et al, Chemonucleolysis in lumbar disc herniation: a meta-analysis SciELO
- Cervical Radiculopathy: Surgical Treatment Options OrthoInfo
- Huang P et al, 2014, How fast pain, numbness, and paresthesia resolves after lumbar nerve root decompression: a retrospective study of patient’s self-reported computerized pain drawing PubMed
- Lindholm RV et al, 1981, The cold foot symptom in sciatica. A clinical and thermographic study PubMed
- Rubinstein SM et al, 2007, A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy PubMed Central
- Fardon DF et al, 2014, Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology The Spine Journal


Bulging and herniated discs can be extremely painful and debilitating conditions that affect many people. These conditions can cause intense pain in the neck and lower back, as well as numbness, tingling, and weakness in the arms and legs. Fortunately, there are treatment options available to help manage these symptoms and improve overall quality of life.
One such treatment option is an epidural nerve block, which is offered by My Premier Pain website. This procedure involves injecting medication into the epidural space around the affected nerve to help reduce inflammation and alleviate pain. Epidural nerve blocks can be an effective option for those suffering from bulging and herniated discs, as well as other conditions such as spinal stenosis and sciatica.
It’s important to note that while epidural nerve blocks can provide relief for many patients, they are not a cure for bulging and herniated discs. Other treatments, such as physical therapy and lifestyle modifications, may also be necessary to fully manage symptoms and prevent further injury.
If you’re struggling with the pain and discomfort of a bulging or herniated disc, My Premier Pain website and their treatment options such as epidural nerve blocks may be able to provide some relief. Don’t hesitate to speak with your healthcare provider to learn more about this and other treatment options available to you.
Hi, My mom was experiencing sharp pain in the right part of her neck, arm , shoulder and numbness in the thumb finger. On consulting the spine surgeon and after examining the MRI CERVICAL SPINE Report (which says and highlighted by the doctor : 1. diffuse disc bulge with right foraminal disc extrusion noted at C5/C6 causing mild compression over spinal cord. Severe narrowing of right lateral recess and neural foramen noted with severe compression over nerve roots. 2. Mild posterocentral disc protrusion noted at C3/C4) he suggested for tablets MYOSPAZ and STEON, combined with phsiotherapy: US/IFT for 10 days including theraband excersices, intensive physio- shoulder and neck. She is following the medication and physiotherapy but the thing is the pain is getting worsened after the prescribed excersices. Can you kindly suggest on this
Hi I have a large bugle st c5 /c6 also small bugle at c4. I have numbness in right thumb and pain and numbness in tips of 2 fingers with pain in middle finger. Pain going down right arm and slightly in left arm. Recently I have pain in right hip could this be related
Bulging cervical discs do not cause hip pain, but when you have bulging cervical discs, you are at higher risk to also have bulging lumbar discs, which can cause hip pain. And of course, there are many other causes of hip pain.
Hi. I am having constant itchy on the bottom of my feet, mostly in my arches. I know it is not topical (been to the dermatologist). I have had a herniated disc at L5 S1 last year. My feet started itchy about 6 months ago. I am sure it is nerve related, but I can’t seem to find any information on it. I do have notalgia paresthetica causing the itching my back, but I can’t find what it is in the feet? The itching is on the feet is similar to the back itching. Thank you in advance.
The itchy feeling in the feet could be related to a herniated disc L5-S1, but I’m not saying it is in your case. Pain, tingling and numbness can go all the way from the lower back to the toes.
On August 11th I had a L5-S1 laminectomy for a herniated disc and spinal stenosis. During the surgery there was a CSF tear which was repaired but continued to leak. After one week a drain was inserted but wasn’t working properly so after 5 days it was clamped off then removed and a stitch put in which stopped the leaking. The back now seems to be healing but since the surgery I have bladder retention and absolutely no bowel control. A follow-up MRI shows a pseudo meningocele but docs say no compression. I am being told time will fix this but after 3 weeks I’m becoming depressed and very concerned.
Any opinion on my situation?
A problem with bladder control in your situation is very likely from the compression of either the spinal cord or a bunch of nerves at the bottom of the spinal cord – the disorder is called cauda equina syndrome. It could be possible that the compression is not very obvious on the MRI. It could be also possible that the spinal cord is not actually compressed but sort of affected by the surgical process or meningocele. What the doctor said was probably from his experience so I can’t comment that. I strongly suggest you to listen your intuition and if the symptoms do not start to improve very soon, go back to the doctor or ask for another opinion. In short: your doctor could be right and the problem will heal on its own, but on the other hand, MRI images are often deceiving and the problem would need additional surgical intervention. I by no means can say or predict what will happen in your case but do not wait too long too seek for additional investigations.
I recently had a bad fall at work MRI shows Bulging disk at T12-L1 and a herniated disk at L5-S1. I have severe pain in left side of my lower back that goes around to the front and down the back of my left leg. I am having bladder issues as well, In April I had a surgery on C5-C7. I have spinal stenosis, degenerative disk disease and osteoarthritis in my entire spine. Will they do surgery on both T-12 / L1 and L5 /S1 at the same time? And would they go through the back or front for the surgery. Lastly what is the recovery time look like?
Contact the surgeon and he will answer these questions – it’s case to case. Lumbar discs are usually operated from the back and the cervical ones from either side. I think you can expect to be at least 2 weeks off work. For symptoms to disappear completely, it may take 1-2 months.
Thank you for the information. But will they do the surgery on both areas at the same time? I am a store manager for a very popular coffe house. I can not return to work until I can be on my feet for 9 hours, lift minimum of 40 pounds, bend over, etc…
I have already had my cervical surgery completed. That was on April 21. I was trying to find out if T1/L1 And L5/S1 would be done at the same time. Also if it would be done through the back or front. This is a workmans comp situation and they have to find a neurosurgeon for me. I can not use my Dr that did my neck due to conflict of interest. I am at the mercy of the Workmans Comp people.
That was meant to say T/12 – L1 and L/5-S1
Yes, it’s likely they will be done the same time.
I recently was involved in a multi-car crash and had to be seen by the ER staff twice. I have had 2 MRI exams. Both show multiple bulges, protrusions, a broad herniation in the lumbar spine and multiple bulges with a herniation of the t12 disc. My issue now is the constant pain, sort of like an intense Charlie-horse, that shoots around my right hip and down into my abdominal and even extends into my right testicle. In the past I’ve had 2 cervical neck fusions and one lumbar spine fusion, at l5,s1. Is there anyone else who has information on the t12 injury that can help.
T12-L1 disc injury is rare but it can cause pains as you described. Herniated discs often heal on their own with time, at lest to some extent. You can ask a doctor if a steroid injection would help relieve pain in your case.
Hello, I just wanted to ask if an altered breathing pattern and nausia can be a direct symptom from cervical stenosis at the C3-C4 level. I had a 3 level fusion at C4 to C7 back in 2009 and then an unsuccessful decompression foraminotomy at C6 and C7 in 2013. It was discovered in 2012 from an MRI that there was a retrolisthesis at C3-C4 with a posterior bulge of 4.3 millimeters. 3 doctors have suggested this was the reason for my cervico genetic vertigo and constant headaches. It has now progressed to the point where just tilting my head backwards or forward causes nausia and an altered deep breathing pattern along with imbalance to develop. My injuries were a direct result of a whiplash injury accident in 2009.
It could be possible. I strongly suggest you to continue your discussion with the doctors.
I have a vibrating feeling in my sacral area mostly when sitting and or flexing my neck. It started about 9 months ago and has stayed with me. It doesn’t seem to get better or worse. I have an extensive history of lumbar back problems. I.e. herniated disc. I’ve never had surgery. I was in a car accident and suffered through Thoracic outlet syndrome and post concussive syndrome. That was about seven years ago. I have had lower back and sciatic nerve pain on a fairly steady basis meaning most every day for the last six or seven years as well so I haven’t been put on a narcotic program for pain relief. But my real concern was only to the new symptom of the nerve vibration in my pelvic region any thoughts?
It’s very likely related to pinched nerves or to spinal stenosis (compression of the spinal cord). I strongly suggest you to visit a neurologist soon.
Hi, I am a 26 year old male. From last 1 month I’m having pain in my left shoulder, neck and hand. MRI report shows.
-)Loss of normal cervical lordosis.
-)C3-4 to C5-6 levels-diffuse disc bulges from C3-4 to C5-6 levels with mild thecal sac indentation and mild impingement of left C4,C5 and C6 nerve roots.
Nisar,
– Loss of normal cervica lordosis means that your neck at the back is not normally bent in as it should be.
– There are bulges in the discs that press on the spinal nerves – so these are pinched nerves that cause pain in your neck and arm.
You need to ask a doctor (a neurologist or orthopedist) what is the best treatment option in your case. I can’t give any general advice, but treatment can be anything from relative neck rest, changing sitting position, a very short-term cervical collar or exercise to surgery.
2 discectomies, ’01-02; fusion L-3/4 in’ 07 and 360 ALIF fusion L-5/S1 in ’14. Now, pain started a wk ago in lower back, around to front, lower groin today, with the start of loose stools but not diarrhea and an increase in previous urinary incontinence In last 2 months accompanied by erectile dysfunction, not severe but has me scared to death. Advice?
Norman, I strongly suggest you to visit a neurologist as soon as possible and ask for a detailed neurological examination. Your symptoms may be due to spinal stenosis or cauda equina syndrome.